World Health Organization (WHO) he declared MPOX constitutes a public health emergency of international concern as a consequence of the increasing variety of cases within the Democratic Republic of the Congo and the potential risk of further spread of the disease.
This is now prompting a coordinated international response to a unprecedented event and resource mobilizationresembling vaccines and diagnostic tests to stop the spread of this infectious disease.
But the WHO has declared mpox a pandemic. Instead, the measures it has triggered are designed to forestall it from becoming a pandemic.
What caused the most recent alert?
Mpox, once generally known as monkeypox, is a viral infection closely related to smallpox. Initial symptoms include fever, headache, swollen lymph nodes, and muscle pain. Then a typical rash appears, mainly on the face, hands, and feet.
The spread of MPox in some African countries has prompted the African Centers for Disease Control and Prevention to declare Earlier this week, mpox declared a public health emergency for mainland security. It is the primary time the organization has issued such an alert since its founding in 2017.
The situation within the Democratic Republic of Congo, in Central Africa, has been particularly worrying for over a 12 months.
There are two types or clades of mpox. Clade II, which originated in West Africa, is less serious. It has a mortality rate of as much as 1% (in other words, about one in 100 persons are expected to die from it). But clade I, originating in Central Africa, has a mortality rate of as much as 10% (up to 1 in ten people die). This is comparable to 0.7% mortality rate for the Omicron variant of the SARS-CoV-2 virus that causes COVID. The Democratic Republic of the Congo is witnessing large outbreaks of the more deadly clade I mpox.
Mpox is endemic in parts of central and western Africa, where the virus occurs in animals and may spread to humans. Outbreaks They grewwith greater spread of disease from individual to individual since 2017
This is partly due to very low level of immunity to the mpox virus, which is said to the virus that causes smallpox. Mass vaccination against smallpox ceased worldwide greater than 40 years ago, leading to minimal population immunity to mpox.
The WHO designation announced this week refers to clade I. Not only does it have a higher mortality rate, but it surely also has recent mutations that increase human-to-human spread. These changes, and a global lack of immunity to mpox, are making the world’s population sensitive to the virus.
There are two different epidemics
In 2022, an outbreak of MPox swept through non-endemic countries, including outside Africa. It was a clade II variant originating in Nigeria, called clade IIb. It was sexually transmitted, affected mostly men who’ve sex with men, and had a low mortality rate.
The epidemic peaked in 2022 when vaccines were made available to at-risk people in high-income countries, but cases surged in 2024.
During the identical period, large clade I epidemics occurred within the Democratic Republic of the Congo, but they attracted much less attention.
There were no vaccines there, even in 2023when there have been 14,626 cases and 654 deaths. The mortality rate was 4.5% and was higher in children.
In fact, most cases and deaths occur within the Democratic Republic of Congo. we were childrenThis means that almost all of the transmissions are non-sexual in nature and are It is probable that it took place through close contact or respiratory aerosols.
Dotted Yeti/Shutterstock
However, in 2023 The outbreak within the non-endemic a part of the country, South Kivu within the east, was almost definitely sexually transmitted, suggesting a couple of epidemic and different modes of transmission within the Democratic Republic of the Congo.
By mid-2024 it was already more cases more within the country than in the entire of 2023 – over 15,600 cases and 537 deaths.
Testing capability within the Democratic Republic of the Congo is restricted, most cases will not be confirmed by laboratory testing, and the info we’ve got come from a small sample of genomic sequences from the Kamituga region in South Kivu.
The clade I virus has been shown to mutate around September 2023 into a variant termed clade Ib, which is more easily contagious between people. We haven’t got much data to match these viruses with the viruses causing cases in the remainder of the country.
Mpox is expanding internationally
Last month the virus It has spread to countries that share a border with the Democratic Republic of Congo – Rwanda and Burundi. It has also spread to other East African countries resembling Kenya and Uganda. Neither of those countries has previously reported cases of mpox.
In a connected, mobile world, cases can spread to other continents, similar to mpox did in 2018. from Nigeria to UK and other countries.
Several travel-related cases that occurred in 2018–2019 could have led to a widespread, multi-country clade IIb outbreak in 2022.
We have vaccines, but not where they’re needed
Because mpoxvirus and poxviruses are related (each are orthopoxviruses), variola vaccines offer protection against mpox. These vaccines were used to manage the 2022 clade IIb epidemic.
However, a lot of the world has never been vaccinated and has no immunity to MPox.
Newer vaccine (called Jynneos in some countries and Imvamune or Imvanex in others) is effective. However, supplies are limited and vaccines are scarce within the Democratic Republic of Congo.
WHO’s declaration of mpox as a public health emergency of international concern will help mobilize vaccines where they’re needed. The African Centers for Disease Control have already begun negotiations to secure 200,000 doses of vaccine, a fraction of what is required to manage the epidemic within the Democratic Republic of Congo.

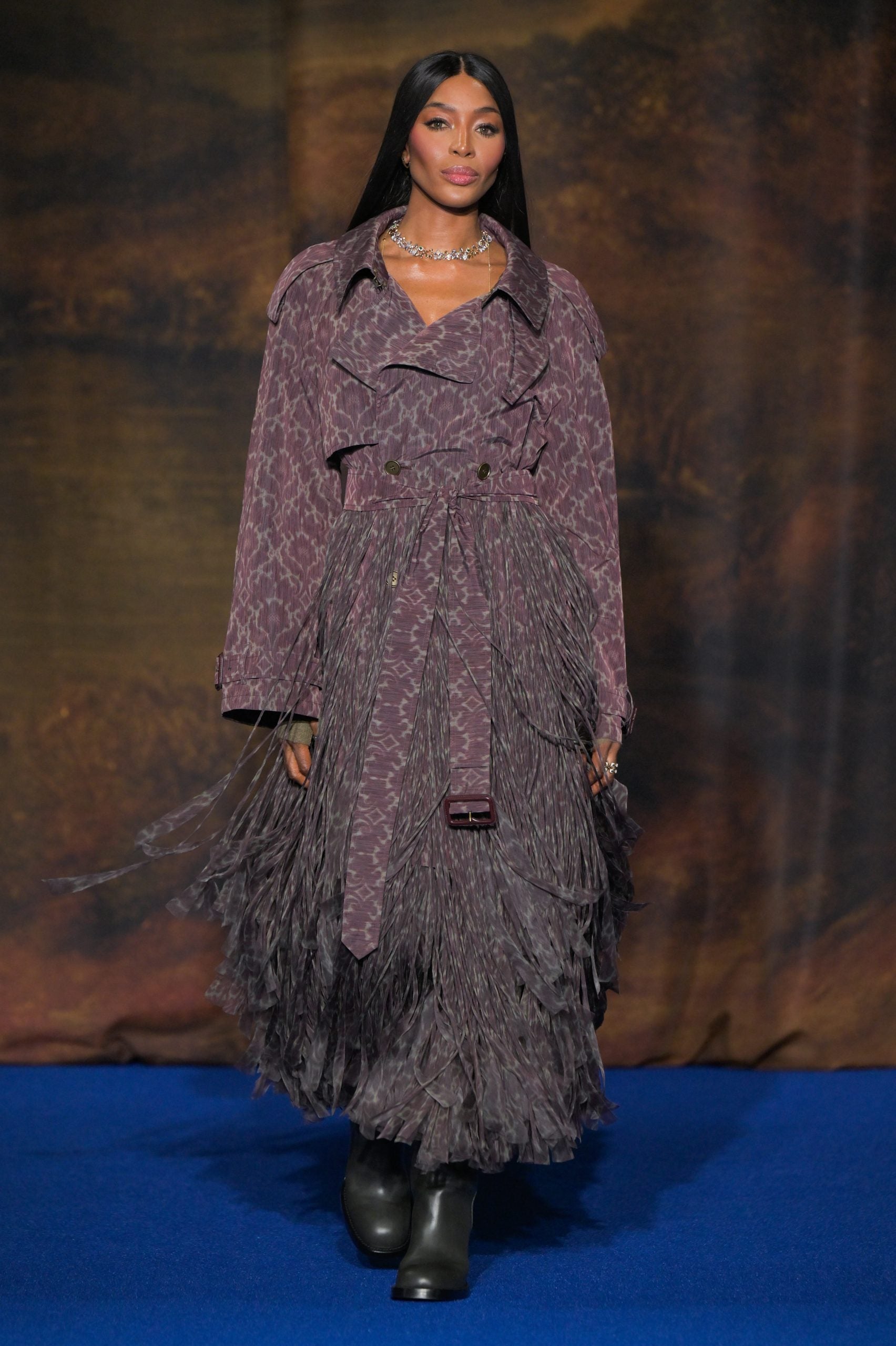
Jeenah Moon/AP/AAP
What will occur now?
Ultimately, a serious outbreak anywhere on this planet is a concern for all of us because it will probably spread globally through travel, as happened with the COVID pandemic.
The best approach is source control, and the most recent WHO statement will help mobilise the needed resources.
Surveillance of the spread of this more serious version of mpox can also be essential, on condition that many countries lack widespread testing capability. We will due to this fact need to depend on “suspected cases,” based on a clinical definition, to trace the epidemic.
Open source software epidemiological interview – resembling using AI to watch trends in rashes and fevers – is also used as an early warning system in countries with weak health systems or delayed reporting of cases.
An additional complication is that 20-30% of individuals with mpox may concurrently have chickenpox, an unrelated infection that also causes a rash. So a preliminary diagnosis of chickenpox (which is less complicated to check for) doesn’t rule out mpox.
Effective communication and addressing resistance to public health measures and misinformation are also key. We saw how vital this was in the course of the COVID pandemic.
Now, WHO will coordinate the worldwide response to the pandemic, with a give attention to equity in disease prevention and access to diagnostics and vaccines. It is as much as individual countries to do what they’ll to follow the International Health Regulations and protocols on how one can manage such a global emergency.