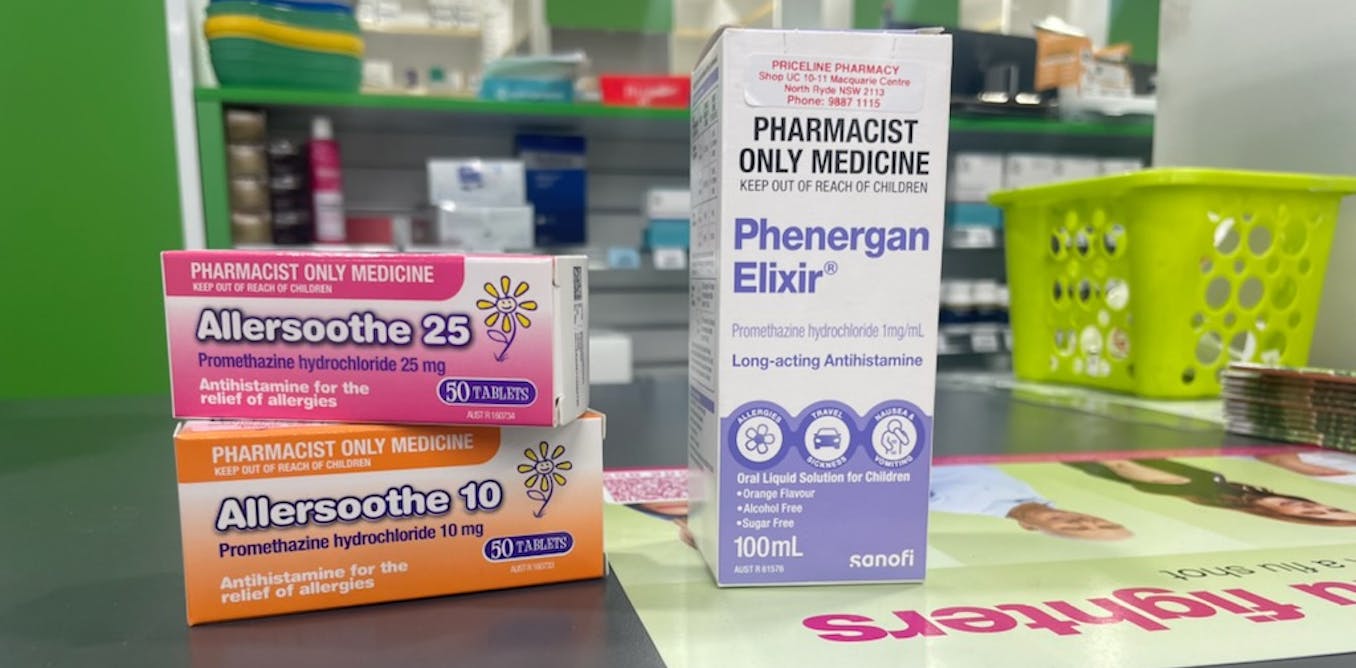
The Australian Drugs Regulatory Authority has issued an order safety warning over Phenergan and related products containing the antihistamine promethazine.
The Therapeutic Goods Administration has stated that over-the-counter products mustn’t be given to children under six years of age due to concerns about serious unwanted effects similar to hyperactivity, aggression and hallucinations. Breathing may additionally change into slow or shallow, which can be fatal.
When high doses are administered to young children, difficulties in learning and understanding, including reversible cognitive deficit and mental disability, may additionally occur. – said the TGA.
The latest warning follows international and Australian concerns concerning the drug in young children, which is commonly used to treat conditions similar to hay fever and allergies, motion sickness and for short-term sedative effects.
What is promethazine?
Promethazine is a “first generation” antihistamine that has been sold over-the-counter in Australian pharmacies for a long time for a spread of conditions.
Unlike many other drugs, first-generation antihistamines can cross the blood-brain barrier. This means they affect your brain chemistry, making you feel drowsy and sedated.
In adults, this will likely be useful for sleep. However, in children, these drugs can cause serious unwanted effects on the nervous system, including those mentioned on this week’s safety alert.
We’ve known about this for a while
We have known concerning the serious unwanted effects of promethazine in young children for a while.
Advice regarding 20 years ago In the United States, the drug was not beneficial for use in children under two years of age. In 2022, an Australian Medicines Advisory Committee made its own suggestion to increase the age to six. New Zealand released similar warnings and advice in May this yr.
Over the last ten years, 235 cases of serious unwanted effects from promethazine have been reported in each children and adults reported to the TGA. Of the 77 deaths reported, one was a toddler under six years of age.
Reported unwanted effects in each adults and children included:
- 13 cases of accidental overdose (leading to 11 deaths)
- eight cases of hallucinations
- seven cases of slow or shallow respiration (leading to 4 deaths)
- six cases of decreased consciousness (leading to five deaths).
TGA security alert comes after an internal investigation by the manufacturer of Phenergan, Sanofi-Aventis Healthcare. This investigation was initiated in 2022 advice from the Medicines Advisory Committee. The company has now updated its information for consumers and healthcare professionals.
What can you use instead?
If you have allergies or hay fever in young children, non-sedating antihistamines similar to Claratine (loratadine) or Zyrtec (cetirizine) are preferred. They provide relief without the chance of sedation and other disturbing unwanted effects of promethazine.
If symptoms of a chilly or cough occur, parents must be reassured that these symptoms will normally subside with time, fluid intake, and rest.
Saline nasal sprays, adequate hydration, a humidifier or elevating the kid’s head can relieve the congestion related to hay fever. Oral products containing phenylephrine marketed for nasal congestion must be avoided because evidence shows that this is the case This article was originally published on : theconversation.com