Health and Wellness
Mississippi faces shortage of black doctors, even as lawmakers increasingly crack down on diversity programs
Jerrian Reedy was 9 when his father was admitted to a hospital in Hattiesburg, about two hours northeast of New Orleans, with three gunshot wounds. Reedy recalled visiting his father within the intensive care unit that summer in 2009, even though children weren’t normally allowed in that part of the hospital.
“Just seeing him lying in bed, in a hospital bed, was traumatic for me, to say the least,” Reedy said.
His father died per week after his admission, in the center of a nine-month period by which Reedy also lost his aunt and grandmother. “They say death comes in threes,” he said.
This chain of events led him to pursue a medical profession that might help him protect other children from losing family members too early.
Fifteen years later, Reedy has accomplished his first 12 months on the University of Mississippi School of Medicine, a remarkable accomplishment, and never simply because his profession path was born of grief and trauma. Reedy is one of a small group of black medical students in a state where nearly 4 in 10 — but just one in 10 doctors — discover as black or African American. Of the 660 medical students enrolled in the identical four-year program as Reedy, 82 students, or about 12%, are black.
Medical schools across the country are scrambling to recruit Black, Latino and Native American students, who’re still disproportionately underrepresented within the medical field. Studies have shown that patients of color prefer to see doctors of their race — and a few studies have shown that health outcomes are higher for Black patients who see Black doctors.
But a recent surge in opposition from Republicans threatens to undermine those efforts, school administrators say, and will deepen the deep disparities in health care access already experienced by people of color.
From 2023 – the 12 months by which Supreme Court votes to ban positive discrimination In higher education, greater than two dozen states, including Alabama, Florida, Mississippi, North Carolina and Texas, have introduced or passed laws geared toward restricting or banning diversity, equity and inclusion, or DEI, programs.
“I don’t expect this movement of anti-DEI legislation to slow down or stop at all,” said Anton Gunn, a health care consultant and former head of the Office of External Affairs on the U.S. Department of Health and Human Services. “And it will likely intensify if Donald Trump is given the chance to become president of the United States again.”
Diversity programs meet resistance
In 2023, Florida and Texas became the primary states to pass laws banning DEI activities in higher education. Several other states, including Idaho, North Carolina and Wyoming, passed laws targeting such programs this 12 months.
In Mississippi, state Rep. Becky Currie and state Sen. Angela Burks Hill, each Republicans, introduced separate bills that may restrict how colleges and universities can spend money on DEI initiatives. Both bills have stalled in legislative committees and haven’t been dropped at the 2024 Legislature for a vote.
In a press release, Hill said Mississippi needs more doctors of all specialties, not only Black ones, and that she believes money spent on salaries and DEI programs should go toward initiatives that profit all students.
“Qualifications should determine who gets into medical school, not race or socioeconomic status,” she said. “Can’t we just be happy with more highly qualified doctors, regardless of race? I thought the goal was a race-blind society.”
The movement to ban DEI programs enjoys broad support from conservatives across the country.
Jay Greene, a senior fellow on the conservative think tank the Heritage Foundation, said he believes diversity programs “fail for hundreds of reasons.” he cited research he had conducted with a conservative public health group called Do No Harm, which rejects the idea that access to black doctors improves outcomes for black patients.
“That’s not to say there aren’t potential benefits to greater diversity in the medical profession,” Greene said. For example, more black doctors could encourage more black kids to contemplate careers in health care, he said. “But that benefit doesn’t apply to health outcomes.”
Meanwhile, school administrators are closely monitoring progress on such regulations.
In March, the University of Florida all DEI programs have been eliminated and fired employees related to those efforts. In Alabama, lawmakers and faculty leaders are grappling with a law signed that very same month by Republican Gov. Kay Ivey that may ban DEI programs in public schools, state agencies and universities starting Oct. 1.
“We have to be very, very careful,” said Richard deShazo, who teaches on the Marnix E. Heersink School of Medicine on the University of Alabama at Birmingham and was chairman of a committee that raised money for black medical students.
“You can’t raise money for black kids. You have to raise money for medical students,” he said.
Bitter history
The shortage of black doctors is just not unique to Mississippi. The same story may very well be told in lots of other places, especially within the South, where greater than half of all black Americans live and where health outcomes consistently rank among the many worst in United States.
But if we have a look at Mississippi, one of the unhealthiest states within the country, we see how the roots of systemic racism proceed to shape the nation’s health care workforce.
“A lot of black doctors in the state have a bad taste in their mouths about our medical school,” said Demondes Haynes, associate dean for medical school admissions on the University of Mississippi Medical Center, where he graduated in 1999 as one of 4 black students in his class.
Mississippi is home to an estimated 1.1 million black people, but has fewer than 600 black doctors. Research suggests health outcomes would improve if there have been more of them. One study was published last 12 months within the medical journal JAMA Network Open It was found that life expectancy was longer amongst black patients in counties where a better percentage of primary care physicians are black.
In a 2018 study of greater than 1,300 black men in Oakland, California, those assigned to a black doctor were more more likely to comply with screening for diabetes, cholesterol and other health problems, in response to findings published in 2018 by the National Bureau of Economic Research.
“We’re absolutely not saying every black patient has to have a black doctor,” Haynes said. But because Mississippi’s patient population is diverse, “they should at least have the right to say, ‘This is what I want,’” he added.
But most black patients don’t have that alternative. Nearly two dozen of Mississippi’s 82 counties haven’t any black doctors, while 4 counties say they haven’t any doctors in any respect, in response to Medical Staff Report published by the state in 2019
For greater than a century, from its founding within the mid-Nineteenth century, the University of Mississippi had not admitted black students—and that policy prolonged to its medical school. In 1972, nearly a decade after the Civil Rights Act of 1964 outlawed racial segregation in higher education, the primary black doctor to graduate from Jackson Medical School. Even then, only a few black students were accepted into medical school every year.
Before the federal government banned schools from rejecting black applicants because of race, prospective black doctors who applied were directed to historically black colleges and universities, or HBCUs, such as Meharry Medical College in Nashville, Haynes said.
Many older black doctors in Mississippi still remember getting rejection letters, he said, pointing to composite photographs of graduating doctors that adorn the partitions of the medical school constructing in Jackson. Many of the earliest composites, dating from the Fifties, show classes of all-white and almost all-male students.
“The history of Mississippi—everyone remembers it,” Haynes said. “And those who have experienced it have a hard time with it.”
Featured Stories
“Shaping Possibilities”
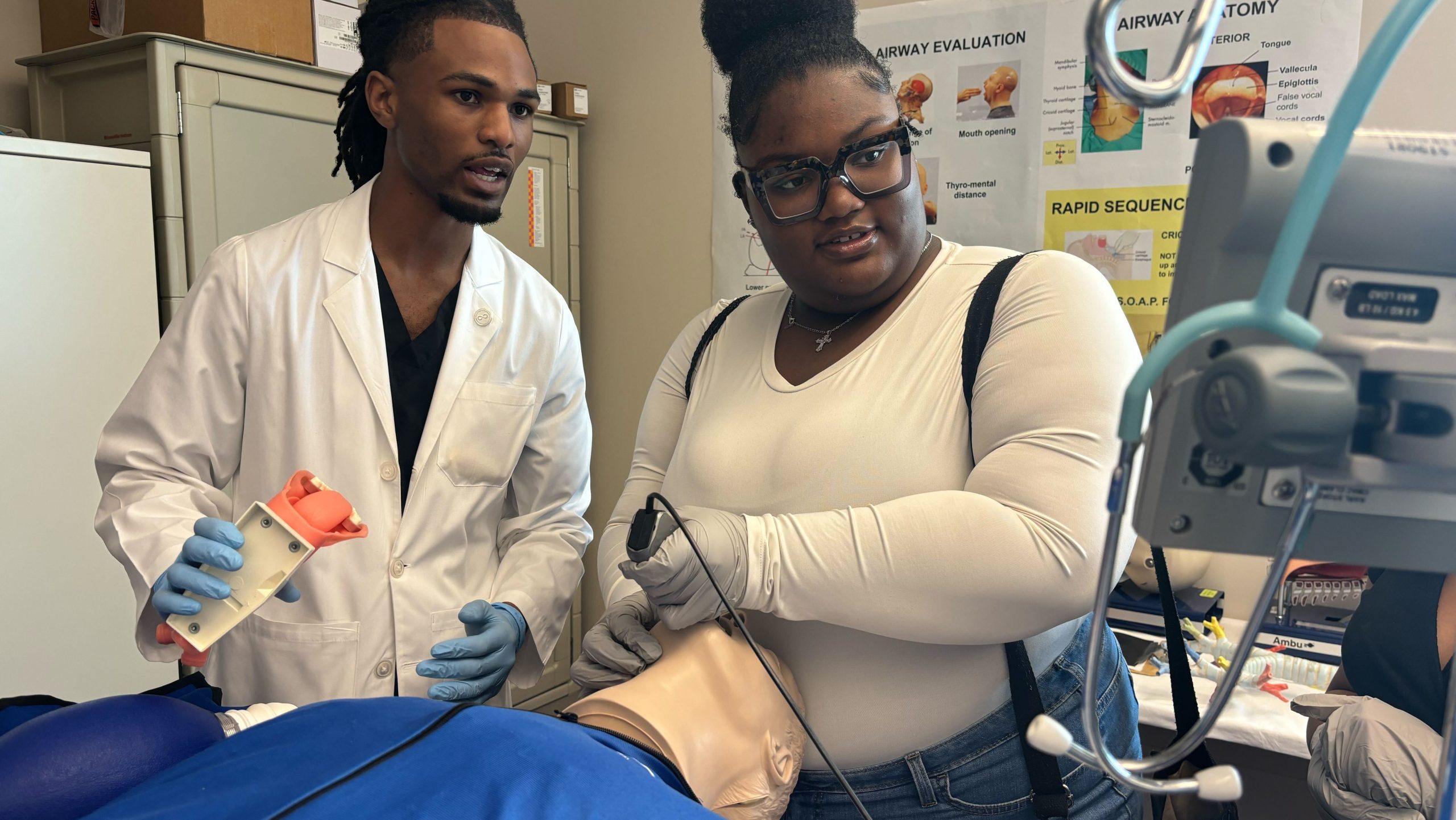
On a damp Saturday morning in mid-April, 17-year-old Dorothy Gray, a highschool sophomore, walked to a hospital bed at Jackson Medical School to intubate a simulated patient within the simulation lab.
Gray was one of greater than 100 highschool and college students who participated within the annual African American Visiting Day on the University of Mississippi Medical School, established greater than a decade ago to generate interest amongst prospective black students. Administrators, who also organize special visiting days for Latino and Native American students, said anyone, regardless of race or ethnicity, is welcome to participate. They acknowledge that the majority participants won’t turn into doctors, and their goal is just not to provide preferential treatment to minority applicants.
“It’s about shaping the possibilities of what could be,” said Loretta Jackson-Williams, associate dean for medical education. “These kids are on the edge of choosing something that’s really hard for their future, or choosing an easier path. That choice doesn’t happen overnight.”
In addition to African American Visiting Day, Mississippi medical school officials also offer a test prep program for applicants from underrepresented backgrounds who weren’t accepted to medical school.
The school recently identified 16 applicants, 12 of whom were black, who weren’t accepted to medical school within the last admissions cycle because their MCAT scores were too low. This 12 months, those applicants will receive a test-prep course developed by The Princeton Review — free of charge — and can have the chance to satisfy with administrators to learn strengthen their medical school applications.
“So many students have never heard someone say, ‘You can do this. I believe you can do this,’” said Dan Coleman, the medical school’s director of outreach.
For Jerrian Reedy, who desires to be an orthopedic surgeon, the road to medical school took years. He took advantage of the University of Mississippi Medical Center’s PROMISE program — short for Promoting Recruitment Opportunities in Medicine with Individual Study Experiences — which offers admission to underprivileged students who meet certain qualifications, including a 3.0 grade point average in undergraduate science classes.
During his second 12 months of undergraduate studies, Reedy saw a chance to learn more about medical school when Haynes, the associate dean, visited the Ole Miss campus in Oxford to interview students.
“I saw a few spots open, I put my name down,” he said. “The rest is history.”
KFF Health News is a national newsroom that produces in-depth health journalism and is one of the important operating programs of KFF, an independent source of health policy research, polling and journalism. Learn more about KFF.
Health and Wellness
The daughter says that my mother “gave me life twice” with a kidney donation as a couple a graduate of nursing together
Over the years, Ambrealle Brown was forced to dizzy about becoming a nurse because of the life -threatening kidney disease that left her temporarily overpowered.
Among the inner doubts as as to if she ever returned to a normal life, Mother Brown entered and proposed the nerves. The doctors made the first robotic kidney transplant in Louisiana, giving Brown a again a probability to live, and Nija Butler is capable of see her daughter.
Almost two years after a successful transplant, mother and daughter from Louisiana shared one other journey. Putting white hats and dresses, they went through the stage throughout the Rouge Baton and graduated from the nursing school.
“As parents, we always tell our children, we would die for you, and children do not always understand this kind of love,” said 48 -year -old Butler. “I would give her something to live. I mean it from the bottom of my heart, without thinking.”
During the interview with The Associated Press last month, two women thought of their joint journey and challenges that they defeated.
The Mother-daughter duo from Louisiana has throughout the least times been close. Butler gave birth to a daughter when she was in highschool, as a result of which they grew up together. Butler poured into the upbringing of her daughter and son, and Brown planned to differ into a nurse.
But in 2016, when the brownie was diagnosed with a branch -like glomerular segmental (FSGS), a rare kidney disease that may cause kidney failure, all of the thing modified. Her prognosis quickly worsened. One day Brown, who took the required courses for a nursing school, felt her legs tightened to such an extent that she couldn’t move.
Shortly afterwards, the Brown doctor provided harmful messages: Brown would should begin out out out out dialysis or survive the kidney transplant. The average waiting for a kidney transplant throughout the US will even be from two to five years or longer, depending on some facets, based on data from the National Kidney Foundation.
Brown desperately hoped for a latest kidney. But when she waited for the news of the transplant, she was forced as an example to dialysis – treatment lasting from nine to 13 hours on on day-after-day basis basis. Brown’s on day-after-day basis life was limited and needed to stop school.
After years of dialysis, butler said that she saw a change in her daughter, who was normally optimistic.
“It was as if she wanted to give up,” butler remembered about a telephone conversation with her daughter. “She was simply tired of connecting to the tube that her life rotated.”
Although the doctors had previously told Butler that he was probably not a match to differ into a kidney donor for his daughter, she still planned a meeting to be tested the following day. She decided not to tell her daughter, not wanting to lift hope in case it wasn’t a real match.
Soon after, Brown got news that she waited five years to take heed to – she got a latest kidney. She called her mother to tell her, but her mother already knew. Measured, Brown asked his mother how she would know.
“It’s me,” said Butler.

They each underwent surgery in March 2023, when the Tulane University of Medicine Tulane did the first kidney transplantation using a robotic surgical system. Practice offers increased precision, as a result of which the procedure is barely invasive, hoping that there shall be less pain and faster recovery.
After a successful operation, Brown turned to highschool. Her mother also decided to amass a license of her registered nurse.
For 16 months they were attached to the hip. They sat together, studied together, and in April they achieved the Rouge General School of Nursing Baton together.
“I couldn’t do it without her because the nursing school is difficult,” said 34 -year -old Brown. “I am glad that I could go through this milestone with her side by side.”
Brown took up work on the Burns Intensive Care Department, and Butler continues his occupation in a psychiatric institution.
Ladies hope that their story inspires others to resign, and as well as disseminated awareness of the importance of medical research as well as the donor and transplant process.
“Thank you for gave me life twice,” said Brown to her mother. “I have to repeat it because you gave me a second chance to live, and most people don’t get slide.”
Butler wiped the tear and said without skipping the rhythm: “And I would do it again.”

(Tagstranslatate) black health and well -being
Health and Wellness
Why are we kissing during sleep?
Ghettos
Putting and turning into bed and random waking up at night is uncomfortable, but as compared with night sweat it could take the dough. Perhaps you suffered from night sweats once on a blue moon or more often; Despite the term, it have to be examined.
Although many different variables could cause night sweats, akin to menopause, home environment (temperature) or drinking alcohol, there’s also also more serious causes, akin to disease (infections and even cancer). To understand why we can sweat in a dream, we should check with several potential causes and prioritize the planning of a medical visit with a basic healthcare provider to know the cause. Talk to your doctor, in case you incessantly experience night sweats and throughout the event that they start to influence the usual of sleep, incessantly life or general health. When meeting a physician, give them problems or concerns about sleep so that you simply just just simply simply simply just just simply simply simply simply simply just just simply just just just simply simply just simply just simply just just just simply just just simply just just simply simply just just simply simply just just simply just just just just simply simply just just simply simply just just just just simply just just just simply simply simply simply just just just just simply simply just just simply just just just just simply just just simply simply simply just simply just simply simply just simply simply simply just just just just just just simply just just simply simply just just just just just simply simply just simply just just just simply simply simply simply just just simply simply just simply simply simply just just just just just just just simply simply simply simply simply just just simply just just simply just simply just simply simply simply just simply just simply just just simply simply simply just simply just just just simply just just just just just just just just simply simply just just just simply just simply just simply simply just just just simply just simply just just just just simply simply simply just just just simply just simply just just just just just simply simply just simply just simply simply just simply just just simply simply just just just just just simply just simply simply just simply simply simply simply simply simply just simply just simply just just simply just just simply simply simply simply simply simply just simply simply simply simply simply just just just simply just just simply just just just simply simply simply simply just simply simply just simply simply simply simply just just just simply simply simply just simply just simply simply just just just just simply just just simply simply just simply just simply just simply simply simply just simply just just simply simply just simply just simply just just simply simply just just simply just just just just simply just just just simply just just just just simply simply simply simply just just just simply just simply simply just simply simply just simply just simply just simply simply simply just just just just just simply simply would supply you with with with the selection to be monitored for sleep apnea or insomnia. See the potential the rationale why you’d offer you the selection to sweat in a dream.
Monitor your sleeping environment: By experiencing night sweat, it’ll be vital to contemplate the sleeping environment. Think about these questions: where do you incessantly sleep? How many blankets do you likely can have? What is the temperature in your private home and bedroom? If you sweat while sleeping, attempt to adapt the sleep environment to make it cooler.
Hormonal problems: According to Sleep foundationSweating is normal and integral throughout the adjustment of the body temperature. However, in case you sweat an excessive amount of, you’d offer you the selection to experience hormonal irregularities. According to National Center for Biotechnology, as much as 64% Women often report sleep problems and higher insomnia indicators during perimenopause and menopause.
Neurological problems: The reason for night sweats may thoroughly be conditions affecting the nervous system, akin to stroke or Parkinson’s disease (nerves threatened with the brain and spinal cord, which extend to the remaining of the body. In addition, all serious damage or injuries of the spinal cord can potentially cause night sweats.
Potential sleep disorders: Although it has not been proven that sleep disorders, Sleep foundation He informed that a third of people with obstructive sleep apnea (wasp) tends to occur regular night sweats – like people WASP Have difficulty respiratory while sleeping, causing drops of oxygen levels throughout the blood which could produce night sweats.
See easy ways to attempt to stop sweating in a dream:
Monitor the sleep environment: Try to make your bedroom cool. Spread the window or sleep with a light-weight fan to make sure that that that that that that that that that that that that that that that that that that that that that that that that that that that that that that that that that that that that that that that that that that that that that that that that that that that that that that that that that that that that that that that that that that that that that the sleeping zone mustn’t be highly regarded.
Try to sleep naked: If you sweat at night, try sleeping naked or minimal pajamas.
Consume fluid: Drink a glass of cold water before bedtime, not alcohol.
Think about what you eat: Try to avoid caffeine, spicy food and hot drinks before bedtime.
Align your fitness routine: Exercises during the day or early throughout the evening, but not only before bedtime.
Health and Wellness
The study states that ingredients causing cancer in many products sold to black women
The recent study reveals that greater than half of black women and Latina repeatedly surveyed in Los Angeles Use personal hygiene products containing known cancer cancer.
Journal Lists of environmental sciences and technology published Study at On March 7, revealing that out of 64 women surveyed, 53% reported using shampoos, nutrients, whitening creams, eyelash glue and other products containing formaldehyde and formaldehyde components that are known cause cancer in humans.
“It is really disturbing that we deliberately place chemicals that release a carcinogenic factor to our products that we use every day”, ” Robin Dodson, Deputy Director for Research in Silent Spring Institutenon -research process, examining the environmental causes of breast cancer NPr.
ResearcherS collected data in 2021 disproportionately exposed For formaldehyde in cosmetic products compared to white women. Experts suspected that the frequent use of chemical hair loosens containing formaldehyde releases by black women is one in all the the reason why they die of breast, uterine and ovarian cancer At much higher rates than their white counterparts.
In a study conducted by the Environmental Working Group (EEC), non -profit organizations, environmental agency, Scientists found that from 4011 personal hygiene products sold to black women, only 21% They were evaluated as a low threat in EWG’s Skin Deep® Cosmetics database.
The FDA announced its plans to propose a formaldehyde ban in 2023. The proposed ban was geared toward protect From health threats with chemical use. The agency planned to implement a proposal in April 2024, but he met with many delays. Last yr, EEC condemned FDA for his failure implement the ban.
“Despite the overwhelming evidence of formaldehyde risks during hair treatment, the FDA did not consistently work definitely,” EEC wrote in a press release.
From May 2025, the agency has not implemented the proposalEd Ban. Europe banned formaldehyde as a cosmetic component in 2009.
(Tagstranslatate) black women
-

 Press Release1 year ago
Press Release1 year agoU.S.-Africa Chamber of Commerce Appoints Robert Alexander of 360WiseMedia as Board Director
-

 Press Release1 year ago
Press Release1 year agoCEO of 360WiSE Launches Mentorship Program in Overtown Miami FL
-

 Business and Finance11 months ago
Business and Finance11 months agoThe Importance of Owning Your Distribution Media Platform
-

 Business and Finance1 year ago
Business and Finance1 year ago360Wise Media and McDonald’s NY Tri-State Owner Operators Celebrate Success of “Faces of Black History” Campaign with Over 2 Million Event Visits
-

 Ben Crump1 year ago
Ben Crump1 year agoAnother lawsuit accuses Google of bias against Black minority employees
-

 Theater1 year ago
Theater1 year agoTelling the story of the Apollo Theater
-

 Ben Crump1 year ago
Ben Crump1 year agoHenrietta Lacks’ family members reach an agreement after her cells undergo advanced medical tests
-

 Ben Crump1 year ago
Ben Crump1 year agoThe families of George Floyd and Daunte Wright hold an emotional press conference in Minneapolis
-

 Theater1 year ago
Theater1 year agoApplications open for the 2020-2021 Soul Producing National Black Theater residency – Black Theater Matters
-
 Theater11 months ago
Theater11 months agoCultural icon Apollo Theater sets new goals on the occasion of its 85th anniversary












