Medical experts recommend antiviral drugs for people aged 70 and over who contract Covid, in addition to for other groups susceptible to severe disease and hospitalization as a consequence of Covid.
However, many older Australians have missed out on antiviral medications after contracting Covid-19. This is one more way the healthcare system fails probably the most vulnerable.
Who missed?
We analyzed COVID-related antiviral use from March 2022 to September 2023 We found that some groups were at higher risk of missing antivirals, including indigenous peoples, people from disadvantaged areas and people from culturally diverse backgrounds and linguistically.
Some of the differences might be as a consequence of different infection rates. However, over these 18 months, many older Australians were infected at the least once, and infection rates were higher in some disadvantaged communities.
How clear are the differences?
Compared to the national average, Indigenous Australians were almost 25% less more likely to be exposed to antivirals, older people living in disadvantaged areas were 20% less more likely to be unwell, and people from a culturally or linguistically diverse background were 13% less more likely to get the disease for antiviral drugs. scenario.
People living in distant areas were 37% less more likely to turn into infected with antivirals than those living in large cities. People from outer regional areas were 25% less more likely to accomplish that.
Grattan Institute
Even inside the same city, the differences are clear. In Sydney, people over the age of 70 from the affluent eastern suburbs (including Vaucluse, Point Piper and Bondi) were almost twice as more likely to be taking antiviral drugs than those in Fairfield in Sydney’s southwest.
Older people in Melbourne’s leafy inner east (including Canterbury, Hawthorn and Kew) were 1.8 times more more likely to be taking the antiviral drug than those in Brimbank (including Sunshine) in town’s west.
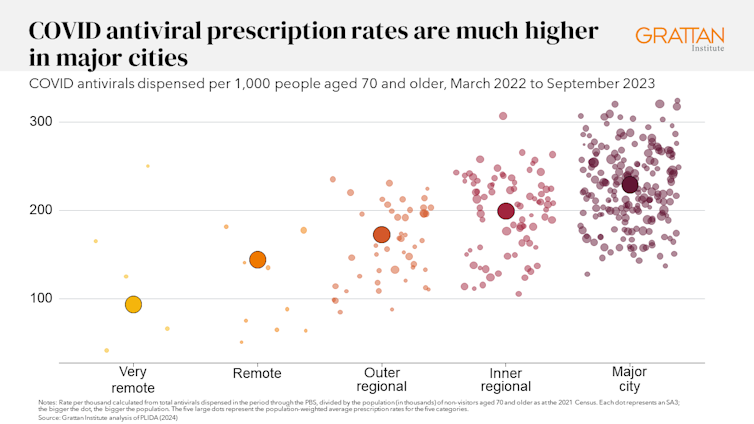
Grattan Institute
Why do people miss?
Antiviral drugs for Covid ought to be taken as soon as the primary symptoms appear. Although awareness about antiviral drugs for Covid is mostly high, people often do not realize they’d profit from the drugs. They Wait until the symptoms worsen and it’s too late.
Frequent visits to your loved ones doctor make an enormous difference. Our evaluation found that folks aged 70 and over, who were more more likely to visit their GP, were significantly more more likely to receive antiviral drugs for Covid.
Regular visits provide a possibility for prevention and patient education. For example, GPs can provide high-risk patients with ‘COVID treatment plans’ as a reminder to get tested and seek treatment as soon as they feel unwell.
Difficulty seeing a GP may help explain the low uptake of antiviral drugs in rural areas. Compared to residents of huge cities, residents of small rural towns have roughly 35% less GPs visit their GP half as often and are 30% more more likely to visit report waiting too long for an appointment.
Just like for Vaccineprimary care physicians’ focus on antiviral medications likely makes a difference, as does ensuring care is accessible to people from diverse cultural backgrounds.
Care should belong to those that need it
Since the period we analyzed, evidence has emerged that raises doubts doubts in regards to the effectiveness of antiviral drugs, especially in people at lower risk of severe disease. This implies that vaccination is more necessary than taking antiviral drugs.
However, all Australians eligible for antivirals must have the identical likelihood of getting them.
These drugs cost greater than A$1.7 billion, with the overwhelming majority of that cash coming from the federal government. Although spending rates have dropped, over 30,000 In August, packages of antiviral drugs for Covid were released, costing about $35 million.
Such an enormous investment mustn’t leave so many individuals behind. Getting treatment mustn’t depend on your income, cultural background or place of residence. Instead, care ought to be targeted at those that need it most.

National Cancer Institute/Unsplash
People born abroad were 40% more likely die from Covid-19 than those born here. Indigenous Australians were 60% more likely die from Covid-19 than non-Indigenous people. And these were people in probably the most disadvantaged situations 2.8 times are more more likely to die from Covid-19 than residents of the richest areas.
Antivirals were more more likely to be omitted for all risk groups.
This is not just an issue with antivirals. These same groups also disproportionately lose access to details about Covid-19 Vaccineincreasing the chance of severe disease. The pattern repeats with other necessary preventive health care measures comparable to cancer film adaptation.
A 3-step plan to satisfy patient needs
The federal government should do three things to fill these gaps in preventive care.
First, the federal government should make primary health networks (PHNs) responsible for reducing them. PHNs, the regional bodies responsible for improving primary care, should share data with primary care physicians and step in to extend service utilization in communities that lack primary care.
Secondly, the federal government should extend it My Medicare reforms. MyMedicare provides general practices with flexible financing for the care of patients who live in aged care homes or often visit hospital. This ought to be the approach expanded all patients, while providing more resources for poorer and sicker patients. This will give GP practices time to tell patients about preventive health care, including Covid vaccines and antiviral drugs, before they turn into unwell.
Thirdly, team prescribing by pharmacists ought to be introduced. Pharmacists could then quickly dispense antiviral drugs to patients in the event that they had previously agreed this with the patient’s GP. This approach would also work for drugs for chronic diseases comparable to heart problems.
Unlike vaccines, antiviral drugs for Covid sustain with recent variants without requiring updates. If a brand new, more harmful variant of the disease emerges, or if a brand new pandemic hits, governments should implement these systems to make sure that everyone who needs treatment receives it quickly.
In the meantime, more equitable access to care will help close big and lasting closures gaps health status between different groups of Australians.