Before the Covid-19 pandemic, the World Health Organization (WHO) did made an inventory priority infectious diseases. They were considered to pose a threat to international public health, but were still needed research to enhance their surveillance and diagnosis. In 2018 “X disease”, which meant that a pathogen we had not previously observed could cause a pandemic.
While it’s one thing to acknowledge the limits of our knowledge of the microbial soup we live in, recent attention has turned to how we’d systematically approach future pandemic threats.
Former US Secretary of Defense Donald Rumsfeld famously talked about “known knowns” (things we all know that we all know), “known unknowns” (things we all know that we do not know), and “unknown unknowns” (things that we do not know that we do not know) .
While this may occasionally have been controversial in the original context of weapons of mass destruction, he asserts a technique to think how we are able to approach future pandemic threats.
Flu: ‘the known known’
Influenza is a largely known disease; Basically, we’ve a minor pandemic every winter with minor variations in the virus annually. However, more severe changes might also occur, leading to spread in populations with little pre-existing immunity. The last time we saw this was in the 2009 case swine flu pandemic.
But there’s much we do not understand about the aspects that drive flu virus mutations, how they interact with population-level immunity, and find out how to best predict transmission risk, severity and impact annually.
The current subtype of avian influenza H5N1 (“bird flu”) spread widely around the world. This led to death many thousands and thousands birds and spread to several species of mammals including cows in the United States and marine mammals in South America.
Human cases have been reported in individuals who have had close contact with infected animals, but fortunately there’s currently no sustained spread between humans.
Although detecting influenza in animals is a big task in a big country like Australia, it does exist on-site systems detecting and responding to bird flu in wild and production animals.
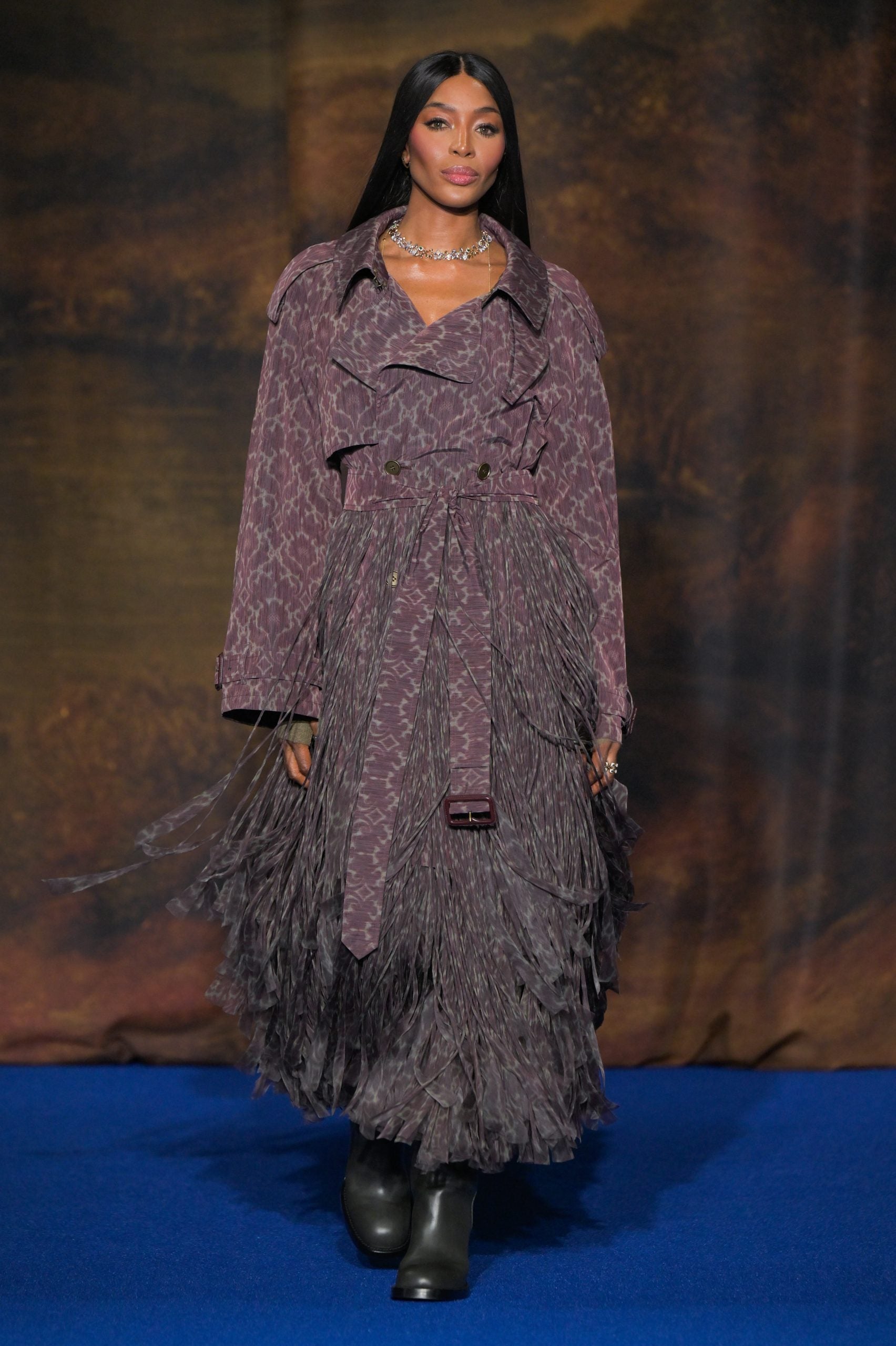
Edward Jenner/Pexels
It is inevitable that there can be more flu pandemics in the future. But it is not all the time the one we worry about.
Attention has been focused on avian influenza since 1997, when the country experienced an avian flu epidemic Hong Kong caused severe disease in humans. But next pandemic in 2009 comes from pigs in central Mexico.
Coronaviruses: ‘the unknown known’
Although Rumsfeld didn’t discuss “unknown unknowns”, coronaviruses would fit into this category. We knew more about coronaviruses than most individuals thought before the Covid-19 pandemic.
We have had experience with Severe Acute Respiratory Syndrome (SARS) and Middle East Respiratory Syndrome (MERS) causing large epidemics. Both are brought on by viruses closely related to SARS-CoV-2, the coronavirus that causes COVID disease. Although they could have disappeared from public awareness before the pandemic, coronaviruses were included in the 2015 list of infections WHO list diseases with pandemic potential.
Previous research on earlier coronaviruses has proven crucial in enabling the rapid development of vaccines against Covid-19. For example, the Oxford group’s initial work on MERS vaccine was key to the development of AstraZeneca’s Covid-19 vaccine.
Similarly, previous research on structure spike protein – a protein found on the surface of coronaviruses that permits them to connect to our cells – was helpful in the development of mRNA vaccines for Covid.
It seems likely that there can be further coronavirus pandemics in the future. And even in the event that they don’t occur on the scale of a pandemic, the effects could be significant. For example, when MERS spread in South Korea in 2015, it caused only 186 cases in two months, but the cost of controlling it was is estimated at $8 billion (A$11.6 billion).

Markus Spiske/Pexels
25 virus families: an approach to ‘known unknowns’
Attention now turned to the known unknowns. There are roughly 120 viruses 25 families known to cause disease in humans. Members of every virus family share common properties, and our immune systems reply to them in similar ways.
An example is flavivirus familythe most famous members of which are the yellow fever virus and the dengue virus. This family includes too several other vital viruses, akin to the Zika virus (which may cause congenital defects in case of infection of pregnant women) and West Nile virus (which causes encephalitisor encephalitis).
WHO epidemic plan goals to contemplate the threats posed by different classes of viruses and bacteria. It examines individual pathogens as examples from each category to systematically expand our knowledge.
The U.S. National Institute of Allergy and Infectious Diseases went a step further by making vaccines and therapies appear on the list prototypical pathogens from key virus families. The goal is to have the opportunity to adapt this data to recent vaccines and coverings in the event of a pandemic brought on by a closely related virus.
Pathogen X, “unknown unknowns”
There are also unknown unknowns, i.e. “X disease” – an unknown pathogen that will cause a serious global epidemic. To prepare for this, we must adopt recent types of surveillance, focusing especially on places where recent pathogens may emerge.
In recent years, there was an increasing recognition of the need for a broader view of health, going beyond fascinated with the health of humans, but in addition of animals and the environment. This concept is generally known as “One health” and takes under consideration issues akin to climate change, intensive agricultural practices, the exotic animal trade, increased human encroachment on wildlife habitats, changes in international travel and urbanization.
This has consequences not only where to look for recent infectious diseases, but in addition how we are able to reduce the risk of disease “spillover” from animals to humans. This may include targeted research animals and folks who work closely with animals. Currently, testing mainly focuses on known viruses, but recent technologies can look for yet unknown viruses in patients with symptoms consistent with recent infections.
We live in an enormous world of potential microbiological threats. While influenza and coronaviruses have a history of causing pandemics in the past, an extended list of latest pathogens can still cause epidemics with significant consequences.
Continued surveillance of latest pathogens, improving our understanding of vital virus families, and developing policies to cut back the risk of virus transmission can be vital to cut back the risk of future pandemics.