Earlier this month, the Government announced significant changes to aged care in Australia, including an A$4.3 billion investment in home care.
In addition to the changes to the home care packages, the home support programme will include a very important addition – the tip of life path for older Australians.
This path offers you access to higher level home care services for older people to assist Australians stay at home as they approach the tip of their life. Specifically, it will provide a further A$25,000 for palliative support where an individual has three months or less to live.
This is a positive change. But there could also be some challenges in implementing it.
Why is this essential?
Older people have clearly expressed their wish to stay of their homes as they age. most individualshome is where they wish to be within the last months of their lives. The space is personal, familiar, and comforting.
However, the information from Australian Bureau of Statistics shows that the majority individuals who die between the ages of 65 and 84 die in hospital, while most individuals aged 85 and over die in residential care homes.
This apparent gap may reflect a scarcity of appropriate services. Both palliative care services and family doctors play a very important role in providing medical care to people living at home with terminal illness. However, the chance die at home is based on the supply of ongoing support, including direct care and assistance with each day living.
Family members and friends often provide this support, but it is not all the time possible. Even when it is possible, caregivers can lack of self-confidence and skills provide the crucial care and should lack sufficient support and respite from their carer role.
Palliative care funding offered by Support at Home should help an older person to stay at home and die at home in the event that they wish.
Unless someone dies suddenly, care needs are prone to increase towards the tip of an individual’s life. Support at home may include assistance with showering and toileting, assessing and treating symptoms, developing care plans, managing medications, dressing wounds, home tasks, preparing meals, and communicating with the person’s family.
Occupational therapists and physical therapists can help select equipment and suggest at-home modifications.
End-of-life support may additionally include explaining goals of care, contacting services corresponding to pharmacists to acquire medications or equipment, liaising with organisations on financial matters, respite care or funeral planning, in addition to accepting grief and offering spiritual care.
However, we don’t yet know what exact services this amount shall be allocated to.
What will we learn about this program thus far?
The in-home support program, including an end-of-life pathway, is scheduled to start on July 1, 2025.
We know that funding is linked to a survival prognosis of three months or less, which shall be determined by a physician.
Further information indicates that the elderly person could also be referred to high priority assessment to access the end-of-life pathway. We don’t know what which means yet, but they don’t need to be current Support at Home participants to be eligible.
The latest path will allow the funds for use over a 16-week period, which is prone to provide some margin of safety with a three-month timeline.
Although an increasing number of details are coming to light, some issues still remain unclear.
Home care providers will want detailed details about what could also be covered by this funding and the way they may work with primary care providers and community health settings.
Older people and their families will need to know what the procedures are for applying for this funding and the way long it will take to process applications.
Everyone will need to know what happens if an individual doesn’t die inside three months.
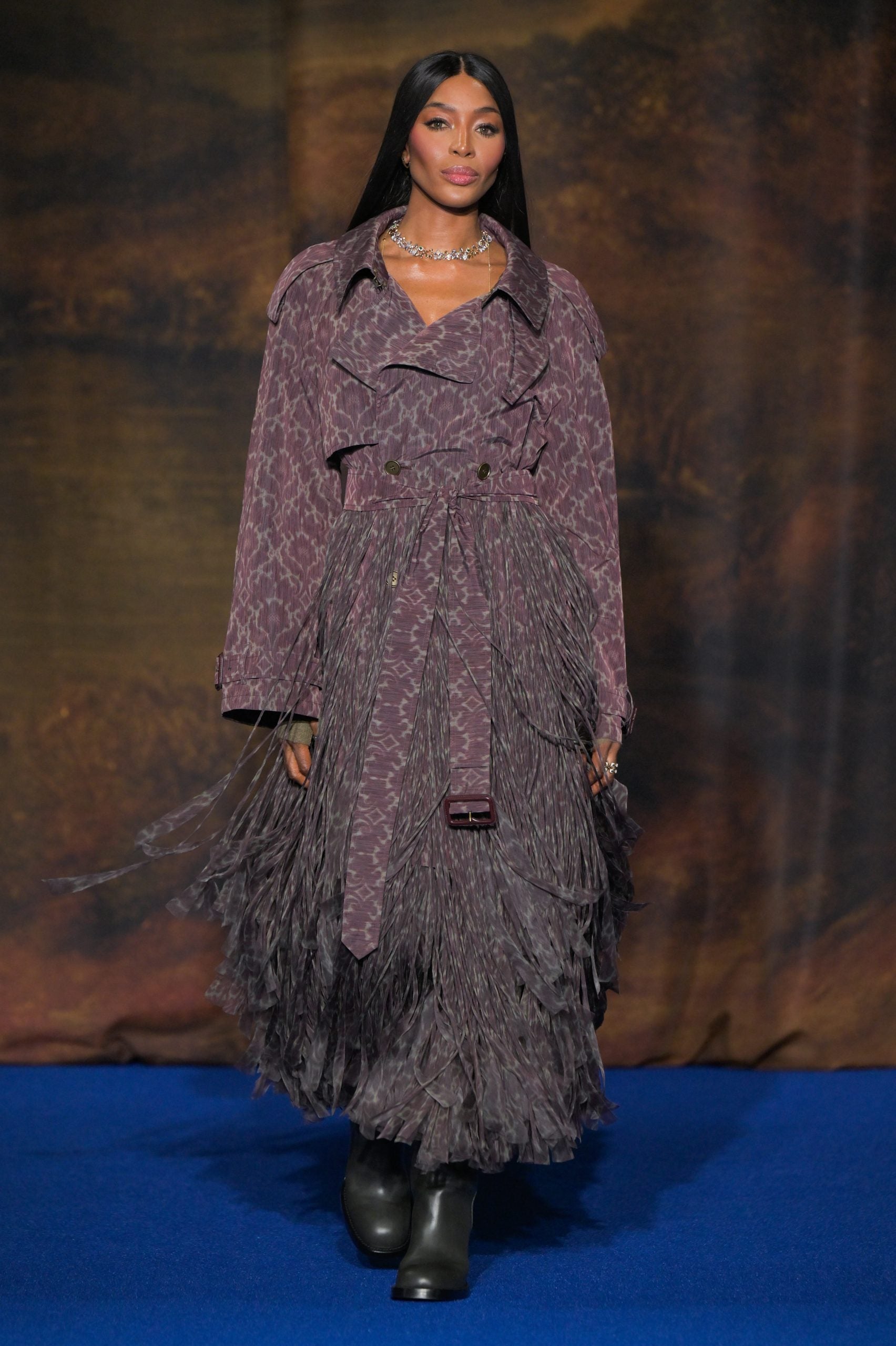
Ground Photo/Shutterstock
Some challenges
The willingness to access appropriate supports and services shall be crucial for older people using this pathway. Home care providers will due to this fact need to evaluate how the end-of-life pathway suits into their operations and the way they can construct the crucial skills and capabilities.
The demand for nurses with palliative care skills and allied medical examiners is prone to increase. Providing end-of-life care can be particularly burdensome It will due to this fact be crucial to develop strategies to stop worker burnout and encourage them to take care of themselves.
It shall be crucial to watch how pathways are implemented in rural and distant areas and across different cultural and social groups to make sure they profit all older people.
Effective coordination and communication between home care, primary care and specialist palliative care providers shall be key. Digital health systems that connect sectors can help. Family involvement may also be very essential.
Escalation and referral pathways must be established to enable appropriate response to emergencies, unexpected deterioration or family distress.
At last, specifying exactly when someone dies can be difficult. Knowing when the last three months of life begin can be difficult, especially when frailty, cognitive issues, and multiple health problems could also be present.
This may mean that some people aren’t perceived as ready for this path. Others will not be willing to just accept this prognosis. The older person may additionally be expected to live with a terminal illness for a lot of months or years. Their palliative care needs won’t be met by this path.
Despite these challenges, the announcement of the Home Care End of Life Pathway is timely and welcome. As a population, we reside longer and dying older. More detail will help us higher prepare for the implementation of this program.