One of essentially the most common feelings related to chronic pain is fatigue, which may grow to be overwhelming. People with chronic pain may report feeling lacking in energy and motivation to interact with others or the world around them.
In fact, a UK study of individuals with chronic health problems found that pain and fatigue were the 2 biggest barriers for an energetic and meaningful life.
But why is long-term pain so debilitating? One clue lies in the character of pain and its powerful influence on our thoughts and behaviors.
Short-term pain can protect you
Contemporary ways of fascinated by pain emphasize its protective properties—the way in which it grabs our attention and forces us to alter our behavior to be able to protect an element of our body.
Try this. Slowly pinch the skin. As you increase the pressure, you’ll notice that the feeling changes until it becomes painful. The pain is what keeps you from squeezing harder, right? It’s how pain protects us.
When we’re injured, tissue damage or inflammation makes our pain system more sensitive. This pain stops us from mechanically stressing the injured tissue while it heals. For example, the pain of a broken leg or a cut under the foot means we avoid walking on it.
The concept that “pain protects us and promotes healing” is one of the crucial vital things that folks with chronic pain tell us. they learned what helped them recuperate.
However, long-term pain can overprotect you
In the short term, pain serves an especially effective protective function, and the longer our pain system is energetic, the more protection it provides.
But persistent pain may also help us prevent recovery. People affected by pain call it “hypersensitivity of the pain system”. Think of your pain system as being on alert. And that is where exhaustion is available in.
When pain becomes an on a regular basis experience, triggered or reinforced by an ever-widening range of activities, contexts, and cues, it becomes a relentless drain on resources. Living with pain requires significant and sustained effort, and this makes us drained.
About 80% of us are lucky enough to not know what it’s wish to be in pain, day in and day trip, for months or years. But take a moment to assume what it’s like.
Imagine having to pay attention hard, gather energy, and use distraction techniques to finish on a regular basis activities, let alone work, caregiving, or other responsibilities.
Whenever you’re feeling pain, you’re faced with a selection of whether and tips on how to act. Continually making that selection requires thought, effort, and strategy.
Mentioning your pain or explaining its impact on every moment, task, or activity is also tiring and difficult to speak when nobody else sees or feels your pain. For those listening, it could grow to be tedious, exhausting, or distressing.
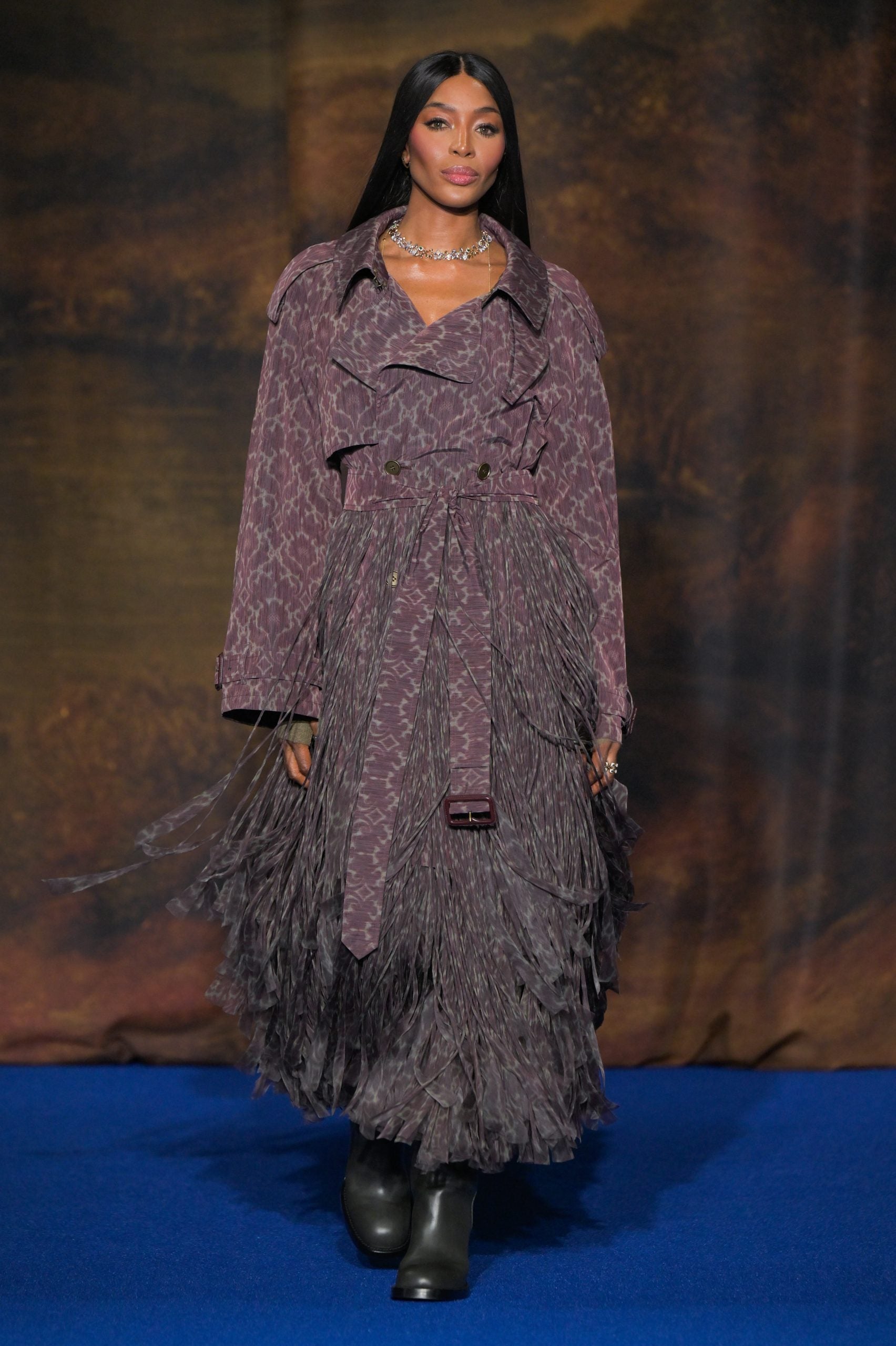
PRPicturesProduction/Shutterstock
No wonder the pain is exhausting
In chronic pain, it’s not only the pain system that’s on alert. Increased inflammation throughout the body (immune system on alert), impaired production of the hormone cortisol (endocrine system on alert), and stiff and cautious movements (motor system on alert) are also hand in hand with chronic pain.
Each of those contributes to fatigue and exhaustion. So learning to administer and resolve chronic pain often involves learning tips on how to best manage the overactivation of those systems.
Losing sleep is also factor each in fatigue and pain. Pain causes sleep disruption, and sleep loss contributes to pain.
In other words, chronic pain is rarely “just” pain. It’s no wonder that long-term pain can grow to be overwhelming and debilitating.
What actually works?
People who are suffering from chronic pain include: stigmatized, rejected AND misunderstoodwhich may result in them not getting the care they need. Ongoing pain can prevent people from working, limit their social contacts and affect their relationships. This can result in a downward spiral of social, personal and economic drawback.
That’s why we want higher access to evidence-based care and high-quality education for individuals with chronic pain.
There is excellent news, nevertheless. Modern chronic pain care, which is based on first gaining a contemporary understanding of the biology underlying chronic pain, it helps.
The key appears to be recognizing and accepting that a hypersensitive pain system plays a key role in chronic pain. This makes a fast fix highly unlikely, but a program of gradual change—perhaps over months and even years—holds promise.
Understanding how pain works, how chronic pain becomes overprotective, how our brain and body adapt to training, after which learning recent skills and techniques to steadily rewire each the brain and body offers hope based on science; there is a powerful supporting evidence With clinical trials.
Any support is helpful
The best treatments for chronic pain require effort, patience, persistence, courage, and infrequently a very good coach. All of this is a fairly overwhelming proposition for somebody who is already exhausted.
So in the event you are among the many 80% of the population that doesn’t suffer from chronic pain, take into consideration what is needed and support your colleague, friend, partner, child or parent on this journey.