COVID-19 vaccines have undoubtedly made an enormous difference during this pandemic. For example, it’s estimated that COVID vaccinations Since their introduction in December 2020, they’ve saved greater than 1.4 million lives in the World Health Organization (WHO) European Region alone.
Unfortunately, SARS-CoV-2 (the virus that causes COVID) is changing quite rapidly, which is affecting how well our immunity from each vaccination and past infection protects us. This problem is usually referred to as “avoiding resistance”.
One strategy to address this issue has been to update our vaccines, which we have now done 4 times in Australia. Now the Therapeutic Goods Administration (TGA) is considering a fifth version of a COVID vaccine – a shot geared toward JN.1 omicron sub-variant.
Here’s what you need to know about these updated amplifiers.
Keeping up with COVID variants
Our first vaccines were directed against the original strain of SARS-CoV-2. first update still in the set original strain but we added an early subvariant of the BA.1 omicron. Then modified BA.1 to BA.4/5 With original strain.
This latest update took place at the end of 2023, after we returned to possession just one ingredient in the vaccine, on this case omicron subvariant XBB.1.5.
The virus continues to change. Another omicron subvariant, JN.1, was first detected in August 2023 and caused a major wave of infections in Australia in the summer.
JN.1 then gave way to other sub-variants that you may know as “Flirt“and the “FLuQE” variants which have been observed relatively large increase in COVID activity in recent months. FLuQE, or KP.3, is currently dominant.
Although JN.1 now not causes many cases, on condition that FLiRT and FLuQE are derived from JN.1, vaccines targeting JN.1 should good job to protect against these newer subvariants.
What is the process?
Already in April, WHO beneficial the use of vaccines against JN.1 line based on the expectation that the virus will proceed to evolve from JN.1. European Medicines Agency issued the same advice.
Potentially, from the point at which it became clear that JN.1 was going to turn into the dominant vaccine, but definitely from that time on, pharmaceutical corporations would have began working to refine their vaccines accordingly.
Once vaccines are ready and tested, they need to be applied to the appropriate regulatory authorities for approval.
The U.S. Food and Drug Administration (FDA) recently approved Emergency Use Authorization regarding Novavax’s vaccine against JN.1.
Meanwhile, the UK regulatory body has approved the JN.1 specification Spikevax by Moderna AND Comirnats from Pfizer.
In Australia our process is barely different and takes somewhat longer. TGA website indicates that applications for 2 JN.1 vaccines are currently under review (Spikevax and Comirnaty). We won’t know after they shall be approved until a choice is made, but we hope it isn’t too far off.
The United States has also approved KP.2 vaccines.
In June, the Food and Drug Administration (FDA) beneficial that vaccine manufacturers: update your COVID vaccines to refer JN.1. However, he later beneficial that it will be higher to use vaccines to combat the KP.2 strain as a substitute (FLiRT).
Moderna and Pfizer have said they’ll find a way to develop vaccines targeting KP.2, and the FDA has given its approval. Emergency Use Authorization for the KP.2 vaccines of those two corporations.
It seems likely that the difference between a JN.1 booster and a KP.2 booster shall be minimal. Both should provide significantly improved protection against the currently circulating subvariants compared with the XBB vaccines. So we shouldn’t feel like we’re missing out by not having plans for KP.2 boosters in Australia presently.
Are the recent vaccines protected and effective?
Before approving updated boosters, regulators are fastidiously analyzing data on the immune response produced by the recent vaccines against newer variants compared with previous vaccines.
Based on data generated mainly by vaccine manufacturers, it seems that the updated JN.1 vaccines lead to significantly improved immune response against multiple related sublineages, including KP.2 and KP.3, in comparison to XBB vaccines.
These latest updates will not be expected to change the well-established security profile COVID vaccines. But as all the time, the safety of vaccines (and their effectiveness) shall be proceed to be monitored even after they’ve been approved and implemented.
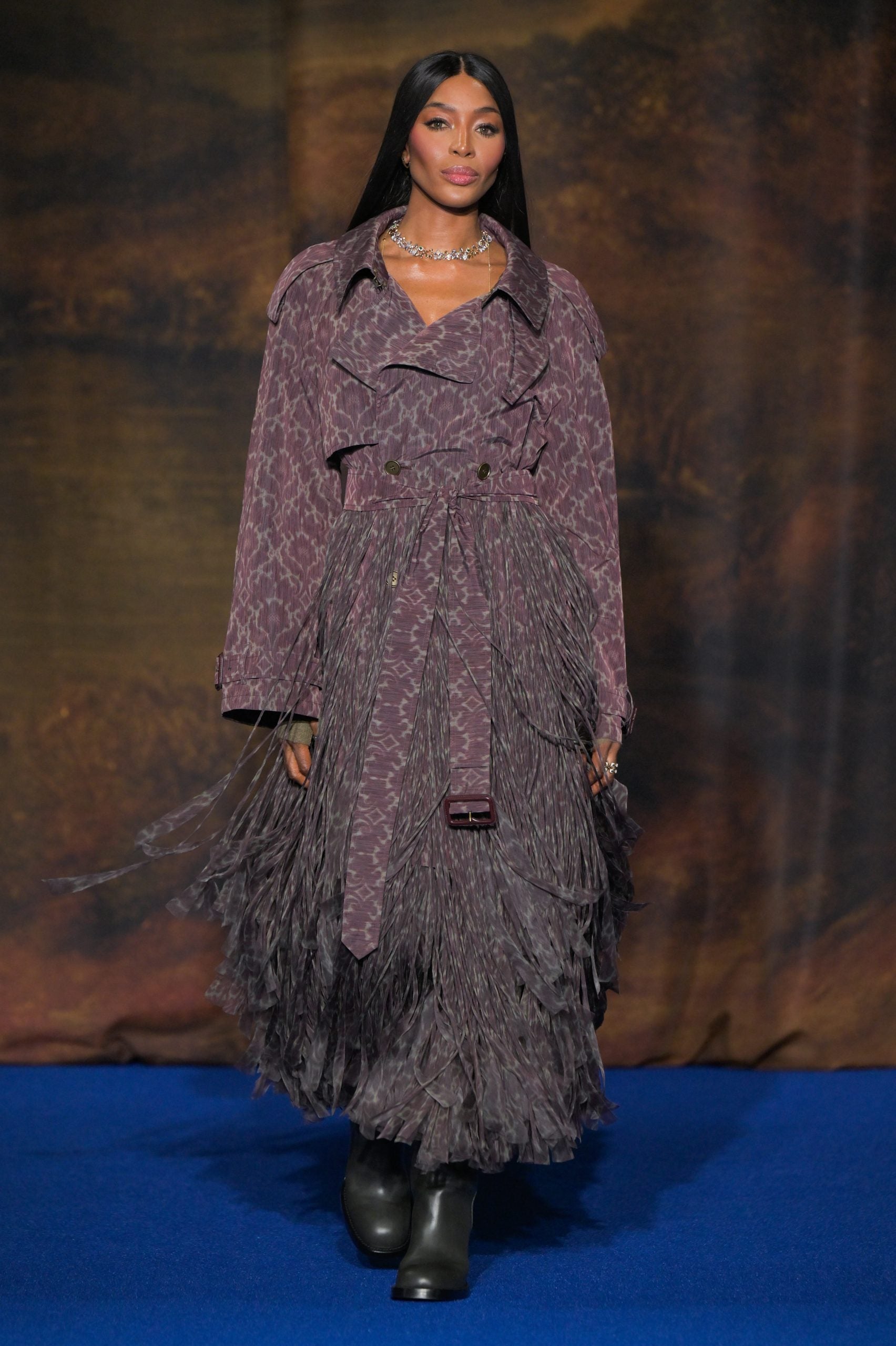
Carlos Giusti/AP/AAP
What about Novavax?
The COVID vaccines from Pfizer and Moderna are mRNA vaccines. They work by instructing our bodies to make the SARS-CoV-2 spike proteins (the proteins on the surface of the virus that it uses to attach to our cells). Then, after we encounter SARS-CoV-2, our immune system is prepared to respond.
This Novavax injection Is adjuvant protein based vaccinemeaning the proteins are produced in a lab, and an ingredient called an adjuvant is added to improve the body’s immune response. Vaccines using this kind of technology have been available for a while, so it’s considered a more traditional way of constructing a vaccine.
While our mRNA options work well, there are individuals who I can not have it or you don’t need an mRNA vaccine, so Novavax provides a vital alternative option.
However, Novavax’s improved booster vaccine doesn’t yet appear to be available to be used before the TGA, so it is probably going to take a while in Australia.
Some challenges remain
While we’re proud to have successfully updated our vaccines, ideally we would really like to develop vaccines that don’t need to be updated as ceaselessly.
But perhaps the most vital consider determining a vaccine’s effectiveness is its uptake, and at once, the rate of individuals getting booster doses of the COVID vaccine is way lower than it must be.
For example, from August only 31.8% of individuals aged 75 and over have received a COVID vaccine in the last six months (beneficial) every six months on this age group).
We also need to look for tactics to approve updated COVID vaccines faster and effectively on this country, including non-mRNA options.