Each time a medication is prescribed in the hospital, the computer will inform the doctor whether the medication is acceptable and what dose to prescribe.
Each time a healthcare provider updates a patient’s medical record on a computer, they have to enter the appropriate information in the appropriate space or select an option from a drop-down menu.
But as a growing group research showsthese electronic systems usually are not perfect.
Our recent study shows how common these technology-related errors are and what they mean for patient safety. They often occur due to programming errors or poor design and have less to do with the healthcare staff using the system.
What were we ? What did we discover?
Our team analyzed greater than 35,000 medication orders at a large urban hospital to understand how common technology-related errors were.
We focused on errors made when prescribing or ordering medications through a computer system. In many hospitals, these systems have replaced the clipboard that hung at the end of the patient’s bed.
Our research has shown that up to one in three medication errors is technology-related. This implies that the design or functionality of the electronic medication system facilitated the error.
We also analyzed how technology-related errors modified over time by examining error rates at three time points: the first 12 weeks of system use and one and 4 years after implementation.
We can expect technology-related errors to turn into less frequent over time as healthcare staff turn into more acquainted with the systems. However, our research has shown that while there may be an early “learning curve”, technology-related errors remained a problem for a few years after the implementation of electronic systems.
In our study, the rate of technology-related errors was the same 4 years after system implementation as in the first yr of use.
How can errors occur?
Errors can occur for a lot of reasons. For example, prescribers could also be faced with a long list of possible doses of a drug and inadvertently select the wrong one. This can lead to a dose that’s lower or higher than intended.
In our study, we found that high-risk medications were often related to technology-related errors. These included oxycodone, fentanyl, and insulin, all of which might have serious unwanted side effects if prescribed incorrectly.
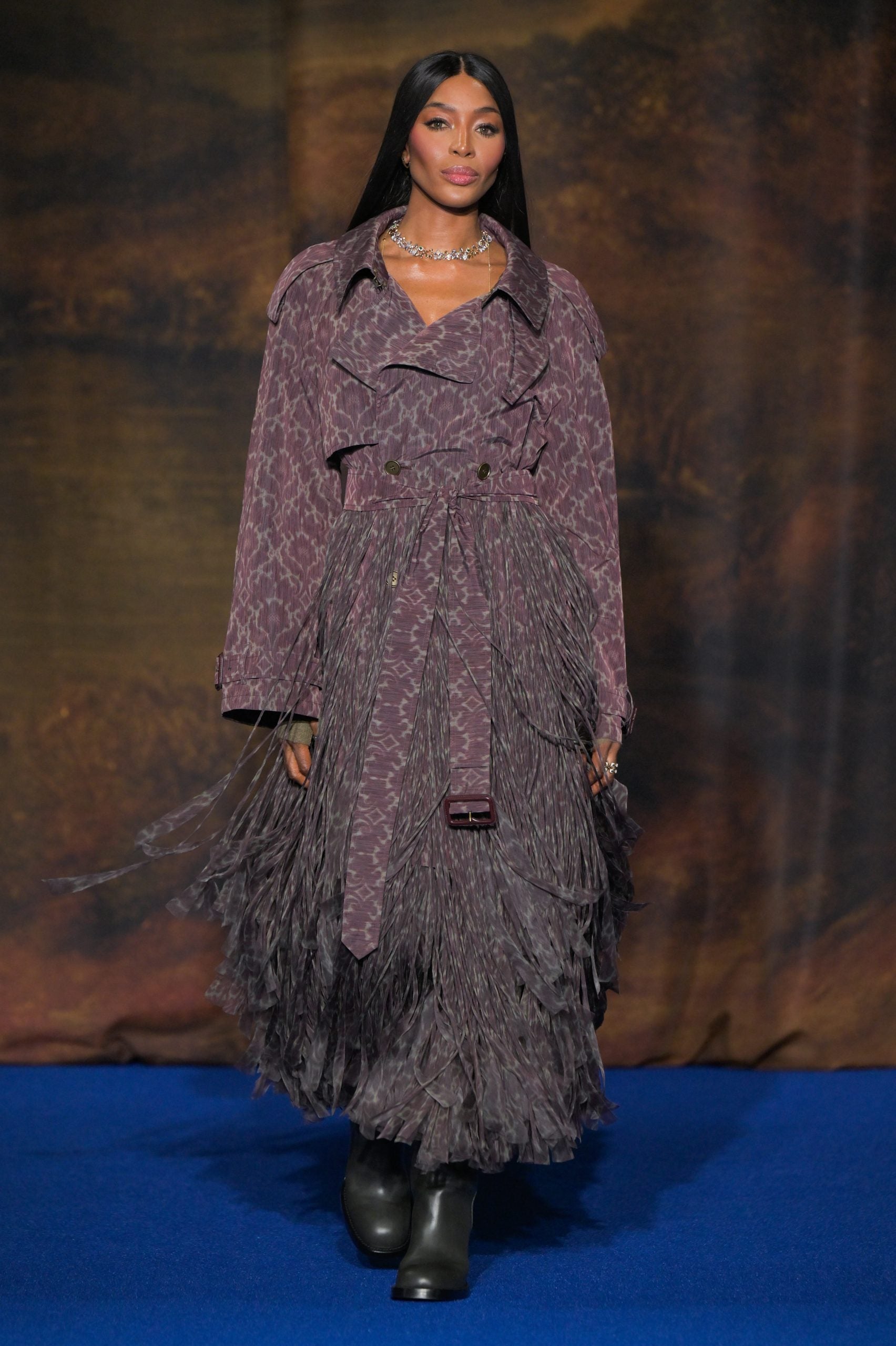
Author provided
Technology errors can occur at any stage of patient care when using a computer.
One case in the United States, a nurse accessed and administered the wrong medication. The medication was taken from a computer-controlled meting out cabinet (generally known as an automatic meting out cabinet) that’s used to store, dispense, and track medications.
Due to poor design, the cabinet allowed the nurse to seek for medications by typing in only two letters. An excellent design wouldn’t have displayed any medication options with only two letters.
A nurse chosen and administered the wrong medication to a patient, which caused cardiac arrest and the nurse faced criminal charges.
Automatic meting out cabinets are used increasingly often rolled out in Australian hospitals.
Earlier this yr we heard about an error in the electronic health records system in South Australia. the payment deadline was calculated incorrectly in greater than 1,700 pregnant women, which can result in premature induction of labor.
We produce a series Security Bulletins for the healthcare system, which describe and address specific examples of poor system design that we have now identified during our research or which have been brought to our attention by others working in the system.
These include a drop-down menu that permits you to prescribe medication via spinal injection. This particular medication could be fatal if served this fashion.
Another one shows built-in calculator which rounds up or down medication doses according to established rules. However, this will lead to incorrect doses in very young or low-weight children.
We provide recommendations for optimizing systems with each example. Organizations can then use these specific examples to test their systems and take motion.
What else could improve security?
As digitalization increases in our hospitals and healthcare, the risk of technology-related errors increases. And that’s before we even start talking about the potential for error in the AI used in our healthcare systems.
We usually are not calling for a return to paper records. But until we tackle the task of constructing computer systems secure, we’ll never fully realize the enormous potential that digital systems can provide in healthcare.
Systems need to be always monitored and updated to make them easier and safer to use and to prevent disasters.
Healthcare IT managers and developers must understand errors and recognize situations where the system design is suboptimal.
Because physicians are often the first to notice problems, mechanisms must be in place to quickly investigate and address their concerns, supported by systematic data on technology-related errors.