It’s cold and wet outside. When you get off the bed, you are feeling it in your bones. Your right knee starts hurting again. It’ll make it harder to walk the dog or go to the gym. You think it should be the weather.
This is a typical belief, but a myth.
When we checked out the evidence, we found no direct link between commonest aches and pains and weather. In the first study of its kind, we found no direct link between temperature or humidity and most joint and muscle pains.
So why are so a lot of us convinced it’s the weather? Here’s what we think is basically happening.
Weather could have a link to health
Weather is commonly related to the risk of recent and ongoing health conditions. For example, low temperatures it might get worse asthma symptoms. High temperatures increase the risk heart problems equivalent to arrhythmia (irregular heartbeat), cardiac arrest and coronary heart disease.
Many people also imagine that the weather is said to their aches and pains. For example, two out of three individuals with osteoarthritis of the knee, hip or hand joints to speak low temperatures cause symptoms.
Musculoskeletal disorders affect greater than seven million Australians. So we decided to examine if the weather is basically the offender behind winter flare-ups.
What did we do?
Very few studies have been specifically and properly designed to search for any direct link between weather changes and joint or muscle pain. And ours is the first to guage data from these specific studies.
We analyzed data from greater than 15,000 people worldwide. In total, these people reported greater than 28,000 episodes of pain, mostly back pain, osteoarthritis of the knee or hip. We also included individuals with rheumatoid arthritis and gout.
We then compared the frequency of pain reports across different weather conditions: hot and cold, humid and dry, rainy, windy, and some combos (for instance, hot and humid versus cold and dry).
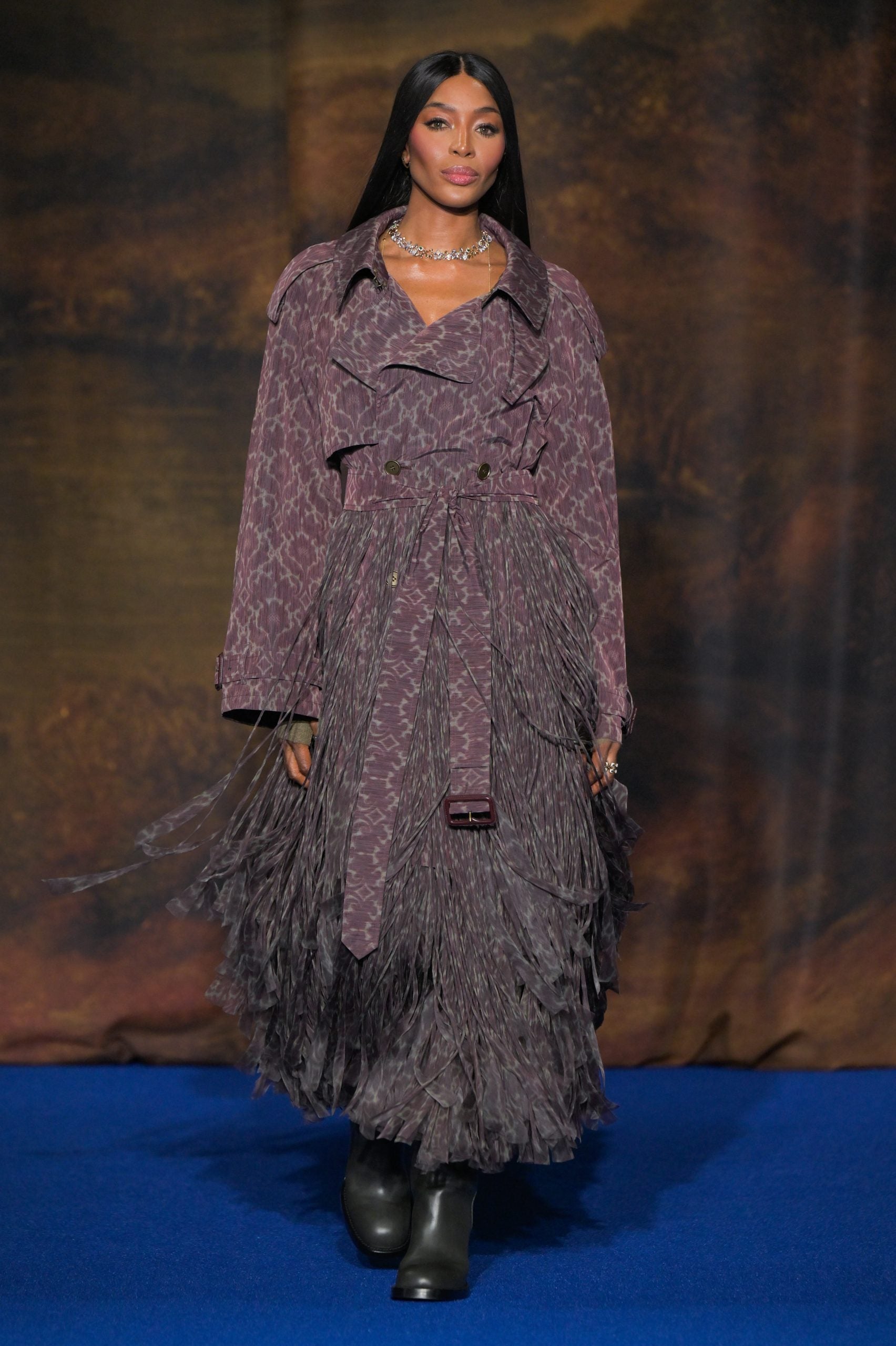
Pearl PhotoPix/Shutterstock
What we found
We found that changes in air temperature, humidity, air pressure, and rainfall didn’t increase the risk of developing knee, hip, or low back pain and weren’t related to people in search of take care of a brand new episode of arthritis.
The results of this study suggest that we do not experience flare-ups of joint and muscle pain consequently of weather changes, and a chilly day doesn’t increase the risk of developing knee or back pain.
In other words, there is no such thing as a link between weather and back, knee or hip pain, nor will it cause arthritis.
It ought to be noted, nevertheless, that very low air temperatures (below 10°C) have been rarely studied, so we cannot draw conclusions about the worsening of symptoms with more extreme weather changes.
The one exception to our findings was gout, an inflammatory type of arthritis that may come and go. Here, the pain worsened in warmer, drier conditions.
Gout has a really different biological mechanism than back pain or osteoarthritis of the knees and hips, which can explain our results. The combination of warm, dry weather may result in increased dehydration and, consequently, increased uric acid levels in the blood and the deposition of uric acid crystals in the joints of individuals with gout, which causes the disease to flare up.
Why do people blame the weather?
Weather can influence other aspects and behaviors, which in turn shape how we perceive and address pain.
For example, some people may change their exercise routine in the winter, choosing the couch as a substitute of the gym. And we know long-term sittingfor instance, is directly linked to worse back pain. Others may change their sleep routine or sleep worse when it’s either too cold or too hot. Again, a nasty night’s sleep can trigger back AND knee pain.
Similarly, mood swings, which frequently occur on cold days, cause a rise in each back AND knee pain.
So it’s the changes in behaviour during the winter that could be causing the pain and discomfort to extend, not the weather itself.
Believing that our pain can be worse in the winter (even when it’s not) also can make us feel worse in the winter. This is generally known as nocebo effect.

Anna Nass/Shutterstock
What to do with winter aches and pains?
It is best to concentrate on pain risk aspects that you would be able to control and modify, moderately than those which are beyond your control (e.g. weather).
You can:
-
Be more physically energetic. This winter and all 12 months round, attempt to walk more, or consult with your doctor about gentle exercises you possibly can safely do at home, with a physical therapist, personal trainer, or in a pool
-
shed pounds in the event you are obese or obese since it is said lower levels joint pain and higher physical fitness
-
keep your body warm in winter in the event you feel muscle tension in uncomfortably cold conditions. Also ensure your bedroom is sweet and warm because we are inclined to sleep less well in cold stores
-
maintain a healthy food plan and avoid smoking or drinking a variety of alcohol. These include key lifestyle recommendations to higher manage many varieties of arthritis and musculoskeletal disorders. For example, for individuals with back pain, a healthy lifestyle is related to higher levels physical function.