Telehealth has been presented as considered one of the solutions to the continued crisis in New Zealand healthcare crisis, which is especially visible in rural areas.
However, moving medical services to the Internet can have a variety of unintended consequences that might affect the well-being of patients and physicians.
Since the pandemic, there was an increasing emphasis on telehealth services – medical visits via online platforms or over the phone. This change in approach is evident in statements regarding government policy concentrate on telehealth options, growth government financing and rapid supplier development.
Telehealth is seen by many as a way to expand access to care, reduce wait times and streamline services. But as my research shows that there are also disadvantages to moving care online. They shouldn’t be ignored.
Advantages and downsides of telemedicine
According to the newest report from 2016, almost 900,000 New Zealanders live in rural areas. Rural Health Network. Their health records could make for grim reading.
The report found that non-Māori men aged 30 to 44 were 1.8 times more likely to die from preventable causes than their peers living in urban areas. And Māori under 30 living in rural areas were twice as likely to die from preventable diseases than their urban counterparts.
As a rural GP in a distant area of Northland, I see the gap in access to healthcare first-hand. For example, there was no everlasting after-hours doctor for 2 years.
Telemedicine has proven to be a support for our patients and a relief for busy doctors.
The positive side is that I not get up 4 times a night to call for help, though I still have to work the subsequent day. And for a lot of patients, talking to a doctor on the phone about a easy matter is way more convenient than traveling 30-40 minutes and waiting in a clinic.
Tests also found that telemedicine might be a viable and culturally protected alternative to in-person consultations for whānau of Māori origin.
However, my tests stated that telemedicine disrupts continuity of care.
Continuity of care, through which a patient maintains a long-term relationship with one physician, has been shown to reduce mortalityThe reduction in mortality with continuity of care is 8% after two to three years and 25% after 15 years.
Putting pressure on other areas
There are many other unintended consequences of telemedicine.
Moving care online or by phone could shift pressure to other parts of the healthcare system. For example, it could increase the burden on rural nurses who’ve to manage highly complex situations without the support of a doctor on site.
A recent case cardiac arrest at Dargaville Hospital Not having a doctor on site should have been a huge challenge for the nurses and an incredibly stressful experience for the whānau.
Tests It also showed how telemedicine can open the door to unsafe medical practices, such as increasing the prescription of the incorrect medications or ordering the incorrect medical tests and studies.
In addition, telemedicine physicians cannot necessarily manage a range of more complex health issues. This finally ends up being passed back to face-to-face physicians to be treated in acute care settings or emergency rooms, increasing the burden on those points of care.
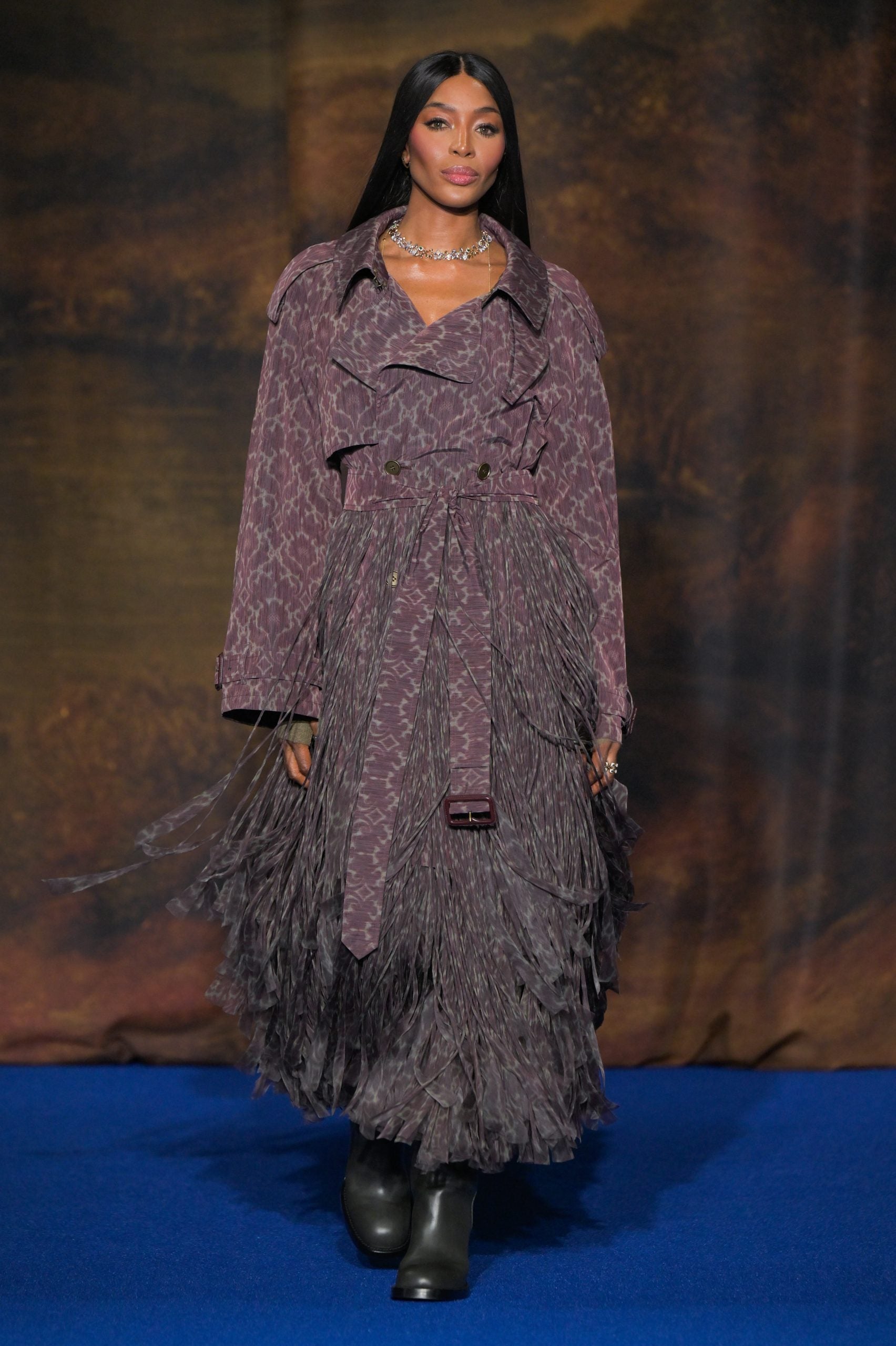
Don Wu/Getty Images
The context is lost
Telemedicine clinicians often don’t live in the identical region as the patient. This means local context and knowledge might be lost.
I even have seen patients who were wrongly referred to a rural hospital after they must have been referred to a larger urban hospital to receive a higher level of treatment.
There is also a more paradoxical problem which will arise: In trying to solve the labor crisis, we are literally making it worse.
Telemedicine providers are recruiting from an already limited pool of doctors in New Zealand. This in turn reduces the general availability of doctors who can provide care face-to-face. It’s easy to see why this is a sexy option for some. Telemedicine positions allow doctors to work at home at hours that suit their lifestyle.
Short-term pondering
In general, rural health solutions don’t seem to be driven by rural labor or rural communities. Rural communities want the identical access to health care that everybody else has.
From 2023 Health NZ has introduced some measures to address the issue of rural healthcare. These include a housing allowance of NZ$9,100 for primary care trainees who live inside 30 kilometres of a rural medical practice, as well as funding for locum GPs, nurses and rural hospital doctors to provide locums in rural general practices and rural hospitals.
However, in rural areas where mortality is high, particularly amongst Māori, there are huge inequalities in access to healthcare and the financial resources needed to close this gap usually are not visible.
The most significant staffing consider reducing mortality, continuity of care under constant physician supervision, doesn’t appear to be taken into consideration in decision-making and policy-making.
Instead, continuity of care is being marginalized by ongoing disruptions to the healthcare sector and the alternative of medical roles with cheaper and easier options – such as telehealth. The government is not specializing in the investment that is required to allow doctors to reach rural areas.
Importantly, solutions to the rural workforce crisis must come from rural communities and rural doctors who’ve the lived experience and know what’s going to really work.