A First Nations baby born in Australia today can expect to live eight to nine years less than a non-native child born on the identical day.
They usually tend to have a heart attack over the course of their lives, and it happens on average 20 years younger than the non-Indigenous patient lying next to them within the hospital bed while they do it. Acute rheumatic fever, a disease virtually unknown amongst non-Indigenous Australians, can damage heart valves. They are more probable get sick and die from cancer, diabetes, kidney failure and lung disease.
A First Nation Australian can be more more likely to have a low household income, live in overcrowded housing, and 14 times more likely be imprisoned. We know that such socioeconomic inequalities cause health inequalities. There can be evidence that cultural aspects and experiences of racism make the issue worse.
Closing the health gap between First Nations people and non-Indigenous Australians is about national priority. One option to reduce health disparities is to enhance the care that Aboriginal and Torres Strait Islander people receive after being admitted to hospital.
Staff at Brisbane’s Princess Alexandra Hospital saw first-hand that our health care system was not providing the care First Nations patients needed. Therefore, they sought to develop a culturally informed model of care for First Nations heart disease patients.
We have all worked with this model and took part in a study to try it out. Our results, recently published in Lancet Global Healthindicate that this culturally based model of care eliminated the gap between First Nations and non-Indigenous patients once we checked out heart health outcomes after they left hospital.
Designing a culturally oriented care model
The model was developed for First Nations patients with acute coronary syndrome. This includes heart attacks and anginathat’s, chest pain attributable to disease of the arteries supplying blood to the heart.
The project was developed collaboratively with First Nations stakeholders. The training was tailored and delivered to construct cultural capability inside the cardiology department and increase staff knowledge of appropriate services available to First Nations patients outside the hospital setting.
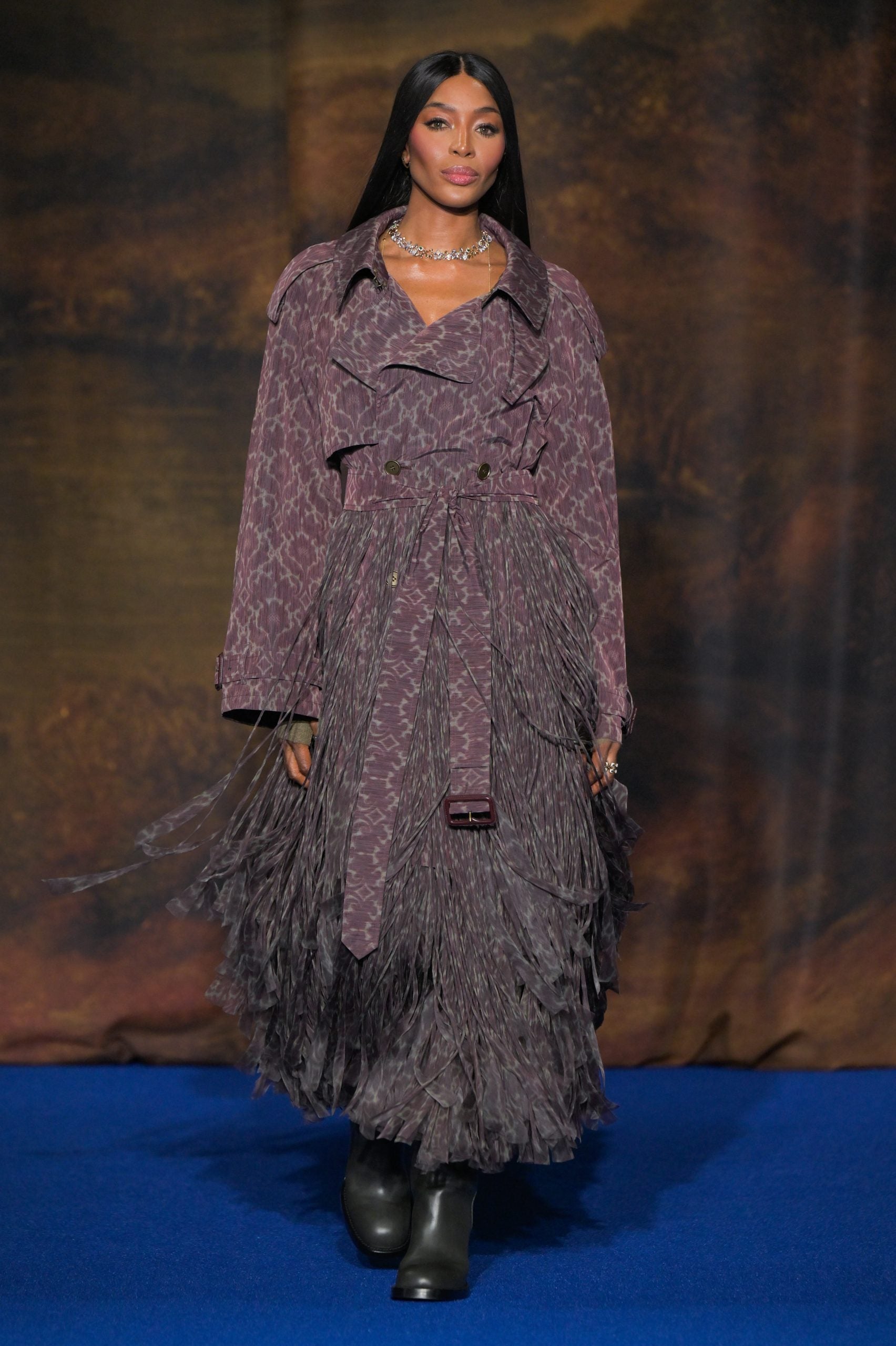
Staff have established formal partnerships with local Aboriginal and Torres Strait Islander community-controlled health organizations. They improved the hospital environment with First Nations art and uniforms (displaying First Nations flags and art).
They assembled a Better Cardiac Care team, which included an Aboriginal and Torres Strait Islander hospital liaison officer, a cardiac nurse and a pharmacist. This team visited First Nations patients at their bedsides, providing additional support, counseling, education and care coordination.
Albert Perez/AAP
Patients could confidently ask questions and talk in their very own words about their diagnosis and treatment, without feeling shame or embarrassment.
The team was focused on the patient’s needs. For example, they may coordinate the accommodation of a patient’s relative who traveled to the hospital from a distance. They could let the doctor know if the patient needed more time to speak or make a decision or a higher explanation. Before the patient left the hospital, the team was capable of liaise with the patient’s local pharmacy to stock his medicines and arrange a follow-up appointment with his GP.
How we tested the model
We examined the impact of the care model by taking a look at outcomes for First Nations and non-Indigenous patients admitted for heart attack and angina before and after implementation of the model.
Specifically, we collected data on 199 First Nations patients and 440 randomly chosen non-Indigenous patients treated within the 24 months before the beginning of the project and compared them with 119 First Nations patients and 467 non-Indigenous patients treated within the 12 months later.
We especially desired to know whether patients died, had one other heart attack, needed unexpected stent or coronary artery bypass surgery, or needed to return to the hospital urgently inside 90 days of discharge.
Before the model was introduced, 34% of First Nations patients had one of these negative outcomes, significantly higher than the 18% of non-Indigenous patients. Subsequently, these events occurred in 20% of each First Nations and non-Indigenous patients. This was a significant improvement for First Nations patients and eliminated the difference between the groups.
The most vital improvement was seen in urgent readmissions, but there have been also fewer heart attacks.

JohnnyGreig/Getty Images
Fewer heart attacks and hospital admissions are good, but we also needed to make sure patients felt culturally secure and had their social and emotional needs met.
AND related project patients and their families were asked about their experiences with the care model. The researchers found that the important thing to success will be the relational or connection between patients and the team, particularly Aboriginal and Torres Strait Islander staff.
A promising concept
Our study was not a randomized trial and the control group was a historical group. It is due to this fact possible that aspects aside from the care model influenced the outcomes. The study was also conducted in just one hospital.
However, we’ve shown that a culturally informed model of care, developed with and for First Nations peoples, can improve clinical outcomes. Better cardiac care programs based on this idea have now turn into widespread other hospitals in Queensland.
We hope that similar results may be replicated in lots of hospitals and other medical specialties, as improving hospital outcomes is one of many essential steps needed to shut health disparities for First Nations people in Australia.