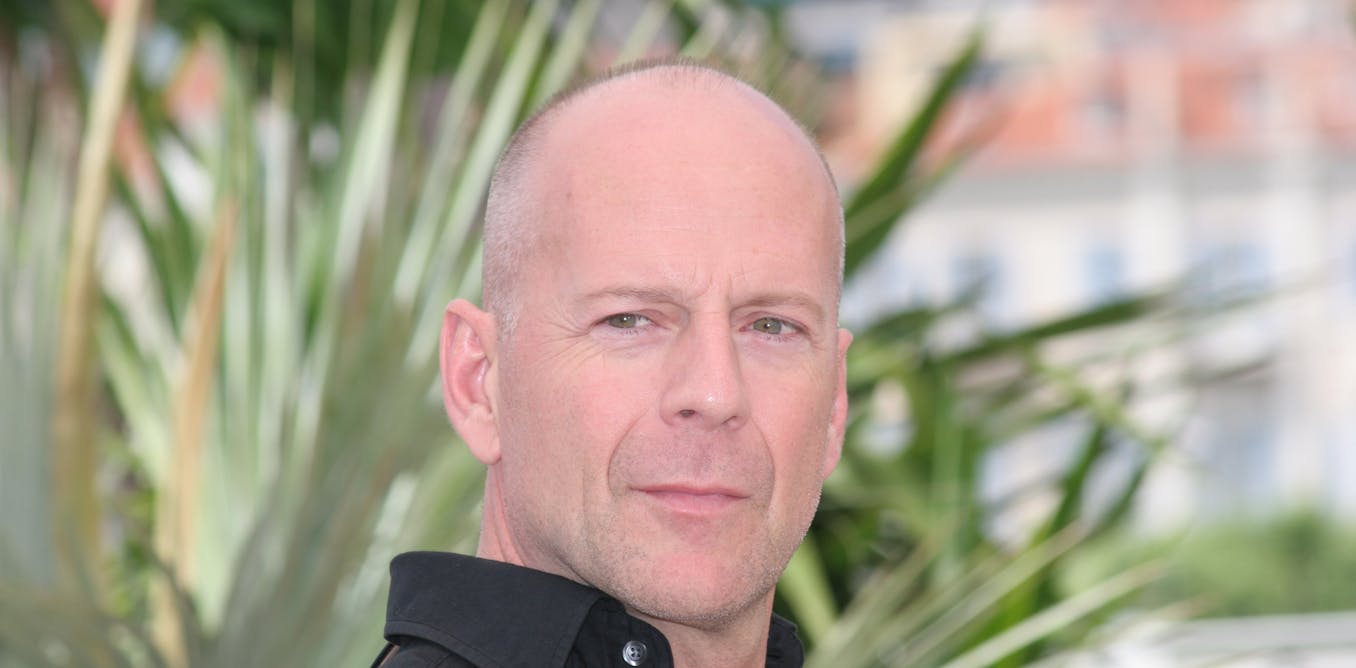
The frontally and defense dementia has gained significant attention in recent years after the actor’s family Bruce Willis announced in 2023 that he was The state was diagnosed. A yr later it was revealed that she was hosting Chat in the USA Wendy Williams The state was diagnosed.
However, despite this recent attention, we still have no idea much about the frontal and protective dementia – including what mechanisms cause certain symptoms and how we will higher detect the signs of the disease. But Our research He discovered brain processes underlying one of the earliest symptoms of the disease. This discovery brings us a step cling to higher diagnosis and treatment of state.
Frontal dementia About 5% of dementia cases. Symptoms often start in the sixties or seventies. The disease primarily affects the behavior, personality and language skills.
The diagnosis of frontally -protective dementia, which distinguishes it from other forms of dementia (equivalent to Alzheimer’s disease), is the early loss of empathy. This often manifests itself as reduced heat and concern for family members. This symptom may be deeply disturbing for members of the family and family members much like the patient. They may feel as if the patient’s personality has modified – and that his efforts to assist and support meet with indifference.
One sec Loss of empathy He was the subject Many research From the scientific community, precise brain mechanisms underlying the loss of empathy in the front -protective dementia remain unclear.
Together with colleagues from the Karolinska Institute, Lund University and Umeå University in Sweden, we conducted a study that was trying Understand how empathy decreases In front -and -protection dementia. We checked out 28 patients with frontal -protective dementia and compared them with 28 healthy people.
To conduct our study, we used a type of brain scanning called functional magnetic resonance imaging (FMRI). During the FMRI scanner, participants checked out the images of hands punctured by the needles. These paintings were contrasted with images affected by Q-tip hand. This is a well -established neuronouki test, which goals to cause a sense of care and suffering as a witness of one other person in pain. We analyzed the brain activity of patients with frontal and protective dementia while viewing images.
In healthy volunteers, the front of the front rims and the hill are the regions of the brain chargeable for monitoring internal body signals (equivalent to pain). These cerebral systems became energetic after they observed paintings in pain.
AuthorIN Author given (without reuse)
But in patients with frontal and protective dementia, activity in these key areas of the brain has been significantly reduced. These reductions were strikingly related to the degree of empathy, which patients showed in their every day lives, as they’re assessed by questionnaires filled by members of the family.
Empathy and brain function
It is often believed that empathy consists of two dimensions. Empathy is the ability to answer the feelings of others (equivalent to their suffering and care). Cognitive empathy is the ability to grasp the intentions of others.
Although each are closely related, they aren’t the same. It is also possible that a person has one aspect of empathy, but not the other. The difference between Two points of empathy You can actually illustrate two psychiatric conditions, anti -social personality disorder and autism.
People who’ve been diagnosed with anti -social personality disorder are frequently good in understanding other people’s intentions and motivations (Cognitive empathy), but he cannot feel emotionally. This can result in disregarding other people. On the other hand, a person with autism often has the ability to emotional empathy, but may not find a way to use for other people’s intentions (Cognitive empathy).
Our study revealed reduced activity in the brain part associated with monitoring the brain of body states, which are frequently used during emotional empathic with one other person. These discoveries emphasize the critical relationship between this brain system and our ability to consider others.
In the light of these findings, the next step in our research is to look at whether and in how the flow of signals of the body needed to create an internal I is modified in frontal and temporary dementia-as it refers to empathy.
Apart from About 30% of cases are geneticThe causes of the frontal and protective dementia remain unclear. Despite intensive efforts from the community, there is no cure. But due to the brave suffering and their families coming forward, consciousness is growing. This is a key continuation.
We hope that understanding how the brain converts empathy into frontal -protective dementia can’t only help improve the diagnosis, but in the future can pave the path of potential treatment that soothes some of the destructive effects of this disease.